New Human Physiology | Paulev-Zubieta 2nd Edition
Chapter 13: Mechanics of Breathing and Lung Disorders
| HOME | PREFACE | TABLE OF CONTENTS | SYMBOLS | SECTION INFO | CONTRIBUTORS | LINKS | CONTACT US |
Highlights
Study_ObjectivesPrinciplesDefinitionsEssentials
PathophysiologyEquationsSelf-AssessmentAnswers
Further Reading
|
|
|
 |
|||||||||||||||||||||||||||||||||||||||||||||||||||||
|
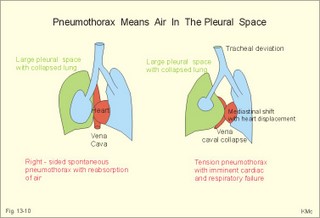
· To define and apply the law of ideal gasses, gas partial pressures and fractions, solubility coefficients, Poiseuille´s and Laplace´s laws. · To describe flow-limitation in the airways, dynamic airway compression, respiratory work, and surface tension (and how it is affected by pulmonary surfactant). To describe obstructive and restrictive lung disorders respiratory failure, cystic fibrosis, and the respiratory distress syndrome in new-borns. · To explain the function of the lung from its structure, respiratory volumes, normal and abnormal airway resistance, static and dynamic pressure-volume relations including compliance, with their measurement and normal values. · To use these concepts in diagnosis, problem solving and apply them to case histories. · The law of conservation of matter (see Chapter 8). This principle is used to measure physiological volumes and volume rates. · The law of ideal gasses is defined in Eq. 13-1 (late in this Chapter). · Poiseuille´s law is used both in the circulatory and the respiratory system (Eq. 13-3). · The law of Laplace (Eq. 13-4). · Bernouille´s principle (Eq. 13-6). · Alveolar ventilation-perfusion ratio (V°A /Q°-ratio) is an estimate of the gas exchange capacity. This key point is the cardinal variable of cardiopulmonary function - see Chapter 14. · Apnoea is a temporary stop in breathing. · Asthma is an inflammatory lung disease characterised functionally by broncho-constriction, hypersecretion and oedema of the bronchial wall - all contributing to obstruction of the airflow. · Chronic bronchitis refers to an inflammatory process in the wall of the bronchioles with excessive production of mucus and sputum from hypertrophic glands. The small airways are narrow, and there is morning cough more than 3 months per year (WHO). · Compliance is an index of expandability of elastic organs and defined as the change in volume per unit change in pressure. · Emphysema refers to destruction of lung tissue distal to the terminal bronchioles (a lung unit termed a primary lobulus or acinus). There is degenerative loss of radial traction of the bronchial walls. · Expiratory reserve volume (ERV) is the volume of air, which can be expired following a normal expiration at rest. · Forced expiratory volume in one second (FEV1) is the 1-s-volume exhaled with forceful pressure from maximal inspiration. FEV1 is often expressed in relation to the total forced expiratory volume (FEV). · Functional residual capacity (FRC = ERV + RV) is the lung volume in the normal end-tidal expiratory position (airways open and relaxed respiratory muscles). · Obstructive lung disorders are characterised by an abnormally low airflow. · Restrictive lung disorders are characterised by small lung volumes (low total lung capacity). · Residual volume (RV) represents the volume of air left in the lungs after a maximal expiration - normally1.2 litre (l) in adult persons. · Solubility (a or Bunsen’s solubility coefficient) is the volume of a particular gas (ml at Standard Temperature Pressure Dry, STPD) dissolved per ml of body warm blood at a partial pressure of one atmosphere (101.3 kPa or 760 mmHg). The solubility coefficients for nitrogen, carbon monoxide, oxygen, and carbon dioxide are listed in Table 13-1. · Spontaneous pneumothorax means that the pleura surface suddenly ruptures without known cause. The rupture typically occurs apically, where the mechanical tension is largest due to expansion. The sudden pain is pleuritic (accentuated by inspiration or coughing), there is dyspnoea, drum sounds by percussion of the affected area and no breath sounds by auscultation. · Total lung capacity (TLC) is the total volume of air in the lungs, when they are maximally inflated (RV + VC) - approx. 6 l of air. · Vital capacity (VC) is the largest volume of air that can be exhaled after a maximal inspiration. VC is measured with or without forced expiration. The size is typically around 4 litres, but it depends on age, sex, and height in the healthy individual.
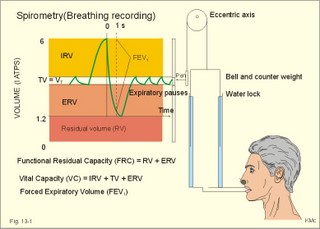
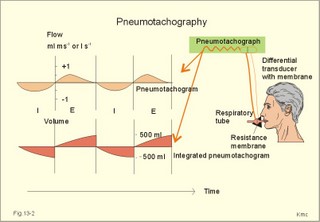
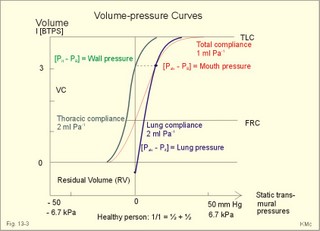
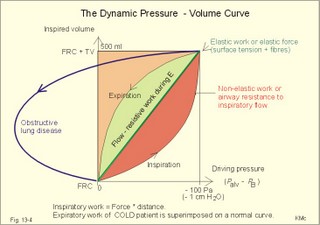
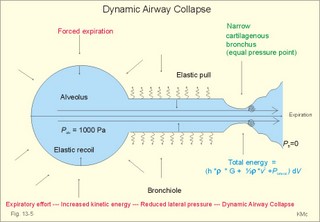
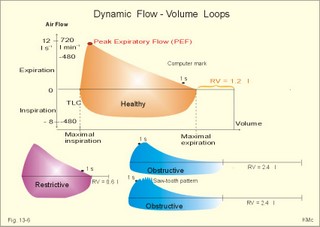
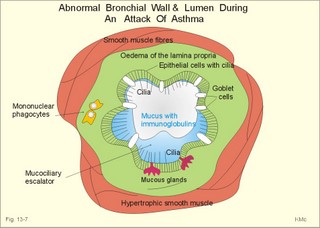
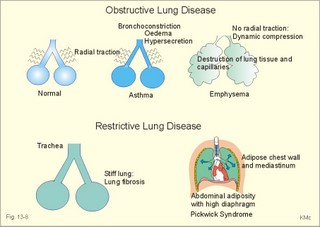
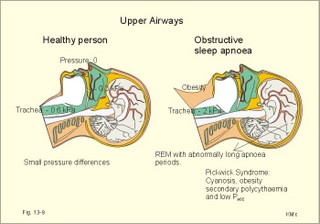
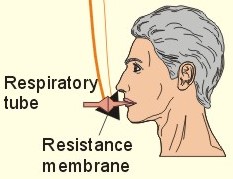
This paragraph deals with 1. Air, 2. Lung volumes, 3. Pneumotachography, 4. The lungs, rib cage and compliance, 5. Dynamic airway compression, 6. Dynamic flow-volume loops, 7. Elastic recoil, 8. Airway resistance, 9. Surface tension, 10. Pulmonary defence mechanisms. Air passes through the nose and mouth further into the airways, where it is warmed, humidified and filtered. From the trachea to the alveoli, there are 23 branching generations of airways. The first 16 (as an average) constitute the conducting zone, which is an anatomic dead space, because no gas exchange takes place. The 17-23 generations form the respiratory zone. Each generation of branching increases the total cross-sectional area of the airways, but reduces the radius of each airway and the velocity of air flowing through that airway. The exchange effective respiratory zone comprises of the respiratory bronchioles, alveolar ducts and alveolar sacs. At this dead end of the airways, there are approximately 300 million alveoli. Each alveolus has a diameter of 100 -300 mm and is surrounded by approximately 1000 capillaries. Each capillary is in contact with several alveoli, so the capillaries present a sheet of blood to the alveolar air for gas exchange. The total area between pulmonary capillary blood and alveolar air ranges from 70-140 m2 in adult humans (increased during exercise) through recruitment of new capillaries in particular in the apical parts of the lungs. Turbulent flow is the agitated random movement of molecules, which accounts for the sounds heard over the chest during breathing. This flow develops at the branch points of the upper airways even in quiet breathing. Turbulence also develops when constriction, mucus, infection, tumours, or foreign bodies decrease the radius of the airways. Vagal stimulation (by smoke, dust, cold air, and irritants) leads to airway constriction, whereas sympathetic stimulation dilatates the airways. Lung volumes are measured by spirometry (Fig. 13-1). A spirometer consists of a counterbalanced bell, which is connected to a pen writing on a rotating drum. The air-filled bell is inverted over a chamber of water, so an airtight chamber is formed. The bell is counterbalanced so it moves up and down with respiration with minimal resistance (Fig. 13-1). Volume changes can be recorded on volume and time calibrated paper. - If the spirometer includes a CO2 absorber, the device is called a metabolic ratemeter (construction Benedict-Krogh). The residual volume (RV) represents the volume of air left in the lungs after a maximal expiration (1.2 l in Fig. 13-1). The vital capacity (VC) is the maximum volume of air that can be exhaled after a maximal inspiration (4.8 l in Fig. 13-1). VC has three components. The first is the inspiratory reserve volume (IRV), which is the quantity of air that can be inhaled from a normal end inspiratory position. The second component of VC is the tidal volume (VT), which is the volume of air inspired and expired with each breath (about 0.5 l at rest). Fig. 13-1: A healthy person, connected to a spirometer, is performing a vital capacity manoeuvre from maximal inspiration to maximal expiration (RV). The third component of VC is the expiratory reserve volume (ERV), which is the amount of air that can be exhaled from the lungs from a normal end-tidal expiratory position that is characterised by a relaxed expiratory pause (Fig. 13-1). This is the easiest position to reproduce, and the lung volume in this position is called functional residual capacity (FRC = ERV + RV). The total lung capacity (TLC) is the total volume of air in the lungs, when they are maximally inflated (RV + VC) - approx. 6 l of air. When the person in Fig. 13-1 exhales with maximal effort, the forced expiratory volume in one-second (FEV1) may be recorded by spirometry. The forced vital capacity manoeuvre is performed with all the expiratory and accessory muscles. When we contract our strong expiratory accessory muscles, we generate high airflows at lung volumes near total lung capacity (Fig. 13-6). Just following peak-expiratory flow (PEF) the airflow velocity decreases linearly with volume no matter how hard the subject tries. This is the effort-independent airflow (Fig. 13-6) caused by dynamic airway compression (see later). A pneumotachograph is a device for measuring airflow. It consists of a respiratory tube with a small resistance (typically a fine network) to airflow (Fig. 13-2). The two chambers separated by the resistance, connects to the differential transducer chambers by thin tubes. – A transducer consists of 2 chambers separated by a membrane, whose position in space reflects the pressure difference. During respiration through the pneumotachograph tube, a small pressure difference (DP) is generated across the resistance, and this pressure difference is directly proportional to the laminar airflow across the resistance according to Poiseuille’s law: Resistance = DP/V°E. Fig. 13-2: Pneumotachograms from a healthy person at rest: The upper curve is the classical flow curve and below is the flow integrated to a volume curve with a tidal volume of 500 ml. 4.The lungs, rib cage and compliance The lung-thoracic wall system consists of two elastic components that work together: The lungs, which behave like a balloon trying to collapse and the thoracic cage trying to expand. The following three important pressures influence the elastic properties of these two components: 1. The barometric pressure (PB). The barometric or atmospheric pressure is one atmosphere and is used as reference pressure. 2. The alveolar pressure (Palv). - The pressure in the alveoli is equal to the static mouth pressure when there is no airflow (during apnoea with the glottis open). The static mouth pressure (= Palv) depends upon the lung volume (Fig. 13-3). 3. The intrathoracic pressure (Pit). - The intrathoracic pressure is the pressure in the fluid-filled pleural space between the parietal and visceral layers of pleura (Fig. 13-3). The intrapleural fluid reduces the friction between the two layers. The Pit can be measured as the pressure in a sensitive balloon, which is passed into the oesophagus. Pressure changes in the intrapleural space equal the oesophageal balloon pressure changes, because the oesophagus traverses the intrapleural space. The Pit is subatmospheric due to the opposing directions of the elastic recoil of lungs and thoracic cage (Fig. 14-5). Fig. 13-3: Transmural, static pressures and lung volumes in a healthy person. – The red compliance curve is for the total system (see later). The blue and green compliance curves are for the lungs and the chest wall, respectively. Compliance is an index of distensibility of elastic organs and defined as the change in volume per unit change in pressure (dV/dP). The following is a description of the measurement of the combined lung plus rib cage compliance, the lung compliance and the rib cage compliance alone. The combined lung plus rib cage compliance The subject expires completely to residual capacity (RV in Fig. 13-3), and then inspires a measured volume of air from a spirometer. The subject then relaxes the respiratory muscles during apnoea while the glottis is open at each volume. The alveolar pressure gradient to the ambient air (Palv - PB) can then be measured as the mouth pressure by a manometer (Fig. 13-3). The procedure is repeated by varying the inspired lung volume between residual volume (RV) and total lung capacity (TLC), and the red relaxation curve of Fig. 13-3 is recorded. This relaxation curve shows the specific standard compliance for the combined system (defined at static conditions as the slope of the curve at functional residual capacity, FRC). In healthy persons, the specific standard compliance for the combined system is 1 ml per Pascal (0.1 l BTPS per cm of water) at FRC. The lungs and chest wall move together and support each other. This is what makes the standard compliance of the combined system less than that of the lungs or rib cage alone (Fig. 13-3). The lung compliance The volume of the lungs before each apnoea is varied in the same way as when measuring the lung compliance for the combined system. The pressure difference between the mouth and intrathoracic (oesophageal) pressure (Palv - Pit) is the blue curve marked transmural lung pressure in Fig. 13-3. In healthy persons, the specific lung compliance is 2 ml per Pascal (0.2 l BTPS per cm of water) at FRC, where the blue lung curve is almost linear (dV/dP at FRC). Normal lungs are very distensible at functional residual capacity (FRC), but stiffen progressively towards total lung capacity (TLC). The falling compliance is caused by an increase in the air-liquid surface tension, because the liquid contains tension-reducing molecules (surfactant, see below) that are spread further and further apart. Thereby the compliance of the lung is reduced. Compliance also decreases with age; there are corresponding decreases in lung volumes. The rib cage compliance This is a calculated variable. The static transmural wall pressure (Pit - PB) is indirectly obtained from the two static transmural pressures measured above. With the two elastic systems in static equilibrium (Pit - PB) must be equal to the difference between the static transmural pressure of the combined system and that of the lungs: (Palv - PB) - (Palv - Pit). According to this equation a minimal increase in lung volume (dV) implies the following relationship: d(Pit - PB)/dV = d(Palv - PB)/dV - d(Palv - Pit)/dV. Each of the entities is an elastance (dP/dV). The elastance of the thoracic cage is equal to the combined elastance minus the lung elastance. The specific compliance of the thoracic or rib cage (dV/dP) is the specific reciprocal elastance, and equal to 2 ml per Pascal (0.2 l BTPS per cm of water). The chest wall compliance curve is constructed by using the above equation (green curve in Fig. 13-3). The driving pressure for air to move is (Palv - PB). The driving pressure and airway resistances are studied when air moves into and out of the lungs, and the condition is therefore called dynamic. The driving pressure for inspiration is a negative alveolar pressure (Palv) relative to PB (Fig. 13-4). Respiratory volume is recorded graphically with a (x, y)-recorder. The tidal volume is plotted against the driving pressure, which is equal to the dynamic alveolar pressure (Fig. 13-4). The resistance to airflow, and the viscous resistance of lung tissue, causes the dynamic pressure-volume curve (Fig. 13-4) to deviate from the static (Fig. 13-3). The slanting straight line (diagonal) is sometimes called dynamic compliance for the combined system (Fig. 13-4). Integrating pressure with respect to volume gives the two green areas corresponding to the elastic work of one inspiration (Fig. 13-4). This is the work needed to overcome the elastic resistance against inspiration. The red area to the right of the diagonal is the extra work of inspiration called the flow-resistive work or alternatively non-elastic work (Fig. 13-4). During expiration, the flow-resistive work is equal to the light green area (Fig. 13-4). The inspiratory and expiratory curve forms a so-called hysteresis loop. The lack of coincidence of the curves for inspiration and expiration is known as elastic hysteresis. With deeper and more rapid breathing the hysteresis loop becomes larger, and the non-elastic work relatively greater. Fig. 13-4: Tidal volume (VT) and the dynamic transmural pressure (Palv - PB) in a healthy person during one respiratory cycle. – The expiratory curve from a patient with obstructive lung disease is shown to the left (see pathophysiology). During a forceful expiration, the intrathoracic or pleural pressure (Pit) rises and causes the alveolar pressure (Palv) to exceed the downstream pressure at the airway openings (PB). As flow resistance dissipates the driving energy along the bronchial tree, the driving pressure of the cartilaginous bronchi falls towards zero at the mouth (Fig. 13-5). At a certain point the forces that expand the airway equal the forces that tend to collapse. This is the equal pressure point. Beyond the equal pressure point the driving pressure falls below the external pressure, and the bronchi are compressed (Fig. 13-5). At this point the person cannot voluntarily increase the rate of expiratory airflow, because increased effort also increases the external pressure. This phenomenon is called dynamic airway compression with airway collapse. The maximum expiratory airflow is effort-independent according to Bernoulli’s law (Fig. 13-6). Bernoulli’s law states that the driving energy equals the sum of the kinetic energy, the constant positional energy and the laterally directed energy (ie, the lateral pressure directed towards the walls). Thus, during expiration the lateral pressure is lowest where the cross sectional area is smallest (the trachea), and the last part of the trachea collapses (Fig. 13-5). Coughing causes momentary collapse of the tracheal wall. The airway closure occurs when the equal pressure point has moved to a part of the airway that is not supported by cartilage and has the smallest cross sectional area (highest kinetic energy). Fig. 13-5: Alveolar sac, bronchiole and a cartilaginous bronchus collapsing during expiration. The peak airway resistance, where flow limitation takes place, is found in the medium-sized segmental bronchi around the 4th-7th generation moving peripherally as lung volume decreases. In healthy people the least resistance to airflow is found in the numerous terminal bronchioles. At low lung volumes the elastic pull in the bronchioles becomes smaller (the structures relax with falling volume) and the airways tend to collapse more easily (Fig. 13-5). Fig. 13-6 shows a dynamic flow-volume loop generated by plotting airflow velocity measured at the mouth with a pneumotachograph against lung volume (integrated airflow velocity). The computer makes a mark after one s of forced expiration. The large loop is from a healthy person performing a forced expiration from full lung inflation (Total Lung Capacity, TLC) to full lung deflation (Residual Volume, RV) that is the vital capacity, VC. This is a so-called forced vital capacity manoeuvre (Fig. 13-6). The inspiratory airflow velocity increases rapidly when inspiring from maximal expiration, and reaches a plateau dependent on muscle force until maximal inspiration, at which point the velocity falls rapidly to zero (Fig. 13-6). Inspiration is limited by the force-velocity relationship of the inspiratory muscles - not flow-limited, as is forceful expiration. Fig. 13-6: Dynamic flow-volume loops for forced vital capacity from a healthy person (yellow area/Residual Volume = 1.2 l). Patients with restrictive (red area/RV 0.6 l) and obstructive lung disease (blue area/RV 2.4 l) are also shown – see pathophysiology. The COLD patient inspires maximally and starts a maximal expiration, but due to the high airway resistance, the flow is abnormaly low causing a 'hammock' curve (Fig. 13-6). The inflammed airways are obstructed by secretion and smooth muscle contraction. The number of airways are reduced as is the pulmonary elastic recoil with loss of alveolar walls and traction causing the airways to collapse. Some patients also have a 'saw-tooth' pattern, due to cardiac contractions. A forced expiration increases both the pleural and the alveolar pressure and the external pressure tend to close the airways. At the point where the airway pressure has fallen due to the flow and is identical with the external pressure, we have the compression or equal pressure point (EPP). An external pressure above this value causes airway compression. Flow is determined by transmural pressure differences at the compression point. The transmural pressure difference is the static expansion pressure of the lung. This is solely dependent of lung volume and stiffness - and independent of increased expiratory strain. Collapse at EPP occurs around the lobar bronchi early during expiration . During further reduction of the lung volume, the airway calliber is reduced and airway resistance decreases (Fig 13-6). This is why the flow-pressure is reduced further and EPP moves to more and more distal airways. Late during forced expiration, the flow is thus determined by the the small airway characteristics. Two forces oppose lung expansion: A. The overall elastic recoil (dP/dV) is the sum of the pulmonary elastic recoil and its surface tension. These forces relate to the elastic work of Fig. 13-4. - Traditionally, the reciprocal elastance or the compliance (dV/dP) is preferred as an index of the distensibility of the lungs and the rib cage. There is a thin fluid layer on the inner surface of the alveolus. Because of the alveolar fluid - air interface a surface tension is created that tends to collapse the alveolus (just like the elastic recoil). The contribution of surface tension to the overall lung elasticity is more than 50%. B. The airflow resistance forces relate to the non-elastic work of Fig. 13-4. The total airflow resistance is the sum of all the resistances of the nose and mouth (a substantial portion of the total) and of the 23 generations of the tracheobronchial tree. The friction between gas molecules and between gas molecules and the walls also contributes to airway resistance. The airway resistance is important and makes the sliding of lung tissue over each other (viscous tissue resistance) a minor issue. In the lungs, the term static compliance is used because the volume and pressure measurements are made when there is no airflow. Increased lung compliance is caused by reduced lung elasticity, and means that lungs with elastic tissue degeneration are easier to inflate. Reduced lung compliance is caused by increased lung elasticity and means that stiff, fibrotic lungs are harder to inflate – see pathophysiology. The driving pressure (DP) for laminar airflow (V°E) through the airway resistance is the intra-alveolar pressure (Palv) minus the ambient or barometric pressure, PB. The airway resistance (Raw) is defined by Poiseuille’s law - see Eq. 13-3. Raw is directly related to the air viscosity (h) and to the length (L) of the tube, and inversely related to its radius in the 4th power: Raw = 8 h L/r4. Doubling the length of the airways only doubles the airway resistance, but halving the radius increases the resistance sixteen-fold. Such a rise in resistance takes place in the small airways during bronchiolitis. The walls of the bronchioles are inflamed causing oedema (swelling), constriction, sloughing of epithelium, and excessive secretion. A similar reversible bronchoconstriction takes place in hyperirritable airway disease (asthma – see pathophysiology). In the clinic the airway resistance is sometimes measured in a body plethysmograph, which is technically demanding to operate, so in everyday clinical practice the Forced Expiratory Volume in 1 second (FEV1) from total lung capacity is used as an indirect measure. This indirect method requires only simple, reliable and accurate spirometers. The patient is asked to expire as fast as possible from TLC by creating a high driving pressure. The driving pressure is considered an arbitrary unit, because it is a reproducible, fast muscle force in each patient. As long as a patient applies an expiratory pressure above the threshold pressure needed to create dynamic airway compression, its absolute size is immaterial. The airway resistance is obtained by dividing the arbitrary expiratory pressure unit by the airflow velocity, FEV1. With increasing lung volume the expanding lung tissue pulls the airways open and thereby decreases the airway resistance. There is a continuum from the top to the bottom of the upright lung, with respect to the degree of airway and alveolar distension. The greatest relative lung distension - at any lung volume - is found at the top due to a more negative Pit. Consequently, the distended top of the lung has the lowest relative ventilation. Thus airway calibre is larger at the top than at the bottom of the upright lung, causing airway resistance to increase progressively from the top to the base of the lung (Fig. 14-5). When the pressure-volume curves in air (Fig. 13-4) are compared to those from saline-inflated excised lungs, it appears that the air-filled lungs are less compliant and show a larger hysteresis loop than when they are inflated with saline. Saline-filled lungs have no air-liquid interface, and thus no surface tension. More than half the total elastic recoil force of the lungs is caused by surface tension. The lungs are suspended in a gravity field tending to separate the parietal and the visceral pleura. The gravity causes the tendency to be greater at the lung apex than at its base. Thus, the intrathoracic pressure (Pit) is more subatmospheric at the apex of the lung than at its base (-900 compared to -200 Pa or -9 to -2 cm of water at FRC). Since the alveolar pressure (Palv) is more or less the same throughout the alveoli, it follows that the transmural pressure gradient (Palv - Pit) over the lung tissue is larger at the apex than at the base of the lung. Therefore, the alveoli at the apex always expand more than the alveoli at the base of the lung. However, the expanded apical alveoli will distend less during inhalation than the small, compliant alveoli located in the middle and basal regions. Pulmonary surfactant lowers the surface tension in the alveoli, which increases the lung compliance. Surfactant is secreted into the thin air-filled interface of the alveolar lining. Surfactant is a complex phospholipid that is a combination of dipalmitoyl phosphatidyl-choline (DPPC) and other lipids and proteins. DPPC orients perpendicular to the air-water interface, such that the charged choline base is dissolved in water (hydrophilic) and the nonpolar, hydrophobic fatty acids projects toward the alveolar air. The type 2 alveolar epithelial cells secrete surfactant. Surfactant prevents alveolar collapse. According to the law of Laplace, the transmural distending pressure in spherical alveoli is equal to T/(2r), where T is the total wall tension (elastic recoil plus surface tension; N m-1) and r is the radius (Fig. 8-9). Because the distending pressure is essentially the same in communicating alveoli, the total wall tension changes with diameter. During expiration the diameter decreases, surfactant molecules are packed tightly together, separating the water molecules and reducing the total wall tension. During inspiration the diameter increases, the surfactant molecules scatter, and the water molecules move closer to each other so the total alveolar wall tension increases progressively; the lung becomes stiffer. 10. Pulmonary defence mechanisms During normal breathing most of the particles of more than 10 mm in diameter - such as pollen - are deposited and removed in the nose and nasopharynx. Particles below 1 mm are deposited in the alveoli. Particles between 1 and 10 mm are deposited in the bronchi - the smaller the particles are the lower they reach. Although sneezing and coughing with expectoration can eliminate many inhaled particles, the mucociliary escalator assisted by bronchus-associated lymphoid tissue (BALT) and alveolar macrophages perform the main clearance of the airways. Mucociliary escalator. The airways are protected by humidification all the way to the alveoli with a mucous layer, which prevents dehydration of the epithelium and surrounds the epithelial cilia (Fig. 13-7). Fig. 13-7: Bronchial wall during an attack of asthma. The protective layer in the lumen is abundant, and consists of a gel phase and a liquid phase surrounding the cilia of the epithelial cells. The lamina propria swells, and the smooth muscle layer is hypertrophic. The airway mucous consists of polysaccharides from goblet cells and from mucous glands in the bronchial wall. Serous and seromucous glands are also active. The mucous forms a gelatinous blanket on top of the liquid layer (Fig. 13-7). The cilia continuously move the gelatinous blanket with inhaled particles on the top upward towards the pharynx, where they are swallowed. Clearance of the respiratory bronchioles may take days, whereas clearance of the main bronchi is typically accomplished within an hour. Smoking reduces mucociliary transport, and indirectly impairs gas exchange. Smoking also reduces surfactant production and thus increases the work of breathing. The lung secretions contain bactericidal lysozyme and lactoferrin from granulocytes. The a1-antitrypsin normally neutralises chymotrypsin, trypsin, elastase, and proteases secreted by granulocytes during inflammation, and thus prevents destruction of lung tissue. Bronchus-associated lymphoid tissue (BALT) in the walls of the main bronchi is part of the mononuclear phagocytotic system or Reticulo-Endothelial-System. These tissue aggregates contain macrophages originating from monocytes and lymphocytes. The lymphocytes are also present in the lamina propria (Fig. 13-7). Following sensitisation of B-lymphocytes to specific antigens, the cells produce specific antibodies or immunoglobulins (IgA, IgG and IgE) in response to new contact with the antigen (Fig. 33-4). IgA inhibits the attachment of poliovirus, bacteria and toxins in the respiratory tract. IgE is related to the pathogenesis of allergic disorders - see Ch. 33. Lungs do have endocrine functions. Alveolar macrophages are amoebic cells that swallow particles and bacteria in the alveoli. While they execute microbes in their phagolysosomes, the cells migrate to the mucociliary escalator, or they are removed by the blood or by the lymphatic system. Smoking impairs the normal macrophage activity. The inactive polypeptide, angiotensin I, is converted into the potent vasoconstrictor, angiotensin II, by the angiotensin converting enzyme (ACE), located on the pulmonary endothelial cells. Angiotensin is important for the regulation of the arterial blood pressure – also during chock. Adrenaline, dopamine, histamine, prostaglandins A1 & A2, prostacyclin (PGI2) and vasopressin (ADH) pass unaffected through the lungs. Bradykinin, leucotrienes, prostaglandins E2 & F2a, and serotonin are almost completely cleared during passage through the lungs by enzymatic activity. Adrenergic sympathetic activity (and sympathomimetic drugs) relax bronchial smooth muscle via adrenergic b2-receptors, whereas parasympathetic cholinergic activity (and parasympathomimetics) constrict bronchial smooth muscles via muscarinic receptors. Smoke, dust and other irritants (perhaps also adenosine, histamine and substance P) constrict the airway smooth muscles via a reflex triggered by the rapidly adapting irritant-receptors (Chapter 16). Decreased PACO2, thromboxane and leucotrienes (see Chapter 32) also act as bronchoconstrictors. Vasoactive intestinal peptide (VIP) can dilatate airways and reduces airflow resistance. Substances that dilatate airways include increased PACO2, adrenergic alpha-blockers, catecholamines and atropine. Lung volumes, as measured with a spirometer, are needed in order to differentiate between two major functional types of lung-airway disorders, and in quantifying the degree of abnormality. The two types are called A. obstructive and B. restrictive disorders (Table 13-2).
The most common disorders are A1. asthma and A2. chronic obstructice bronchitis and emphysema. A special condition called cystic fibrosis is also dealt with. These disorders are all characterised by low expiratory airflow as measured by low Forced Expiratory Volume in one s (low FEV1). The low FEV1 is due to narrowing of the airways with increased airflow resistance. The patient with obstructive lung disease has a smaller flow-volume-loop than that of a normal subject - performed as a forced vital capacity manoeuvre (Fig. 13-6). The RV of the patient is 2.4 l or twice as high as that of the healthy individual, because of air trapping (a large volume of trapped air). Sometimes the so-called saw-tooth phenomenon is observed (Fig. 13-6). This is an unspecific sign of intrathoracic airflow limitation neither related to obstructive sleep apnoea nor to body mass index (Chapter 20). Although the flow-volume curve in obstructive lung disease is consistently reduced in the flow direction, it is not always reduced in the total volume direction (Fig. 13-6). Attacks of asthma occur acute and episodic, but the underlying cause is a chronic inflammation of the lung airways. Asthma is characterised by expiratory airflow limitation due to hyperactive bronchi with eosinophilic inflammation, mucous hypersecretion and bronchoconstriction. Asthma is diagnosed when there is an improvement of FEV1 greater than 15% following inhalation of broncho-dilatators. If necessary, airway hyperreactivity can be demonstrated by histamine or metacholine provocation of bronchoconstriction. Large numbers of eosinophils are present in the sputum, and often in the blood. Skin-prick tests often identify extrinsic causes, which the patient must avoid. Stimulation of the vagal nerve or metacholine provocation causes a forceful reflex bronchoconstriction in asthmatics. This probably explains the hypersensitivity to non-specific stimuli (eg, exercise, cold air or water, pollution, dust, vapours and fumes). Fig. 13-8: Asthma is an acute obstructive lung disease, with reduced lumen due to broncho-constriction, hypersecretion and oedema of the bronchial wall. Emphysema is a chronic obstructive lung disease with degenerative loss of radial traction of the bronchial walls. Diffuse lung fibrosis is characterised by the thick and stiff alveolar interstitium all over the lung. The Pickwick Syndrome is a restrictive lung disorder due to obesity. Asthma occurs in the form of extrinsic asthma, which is caused by a specific allergen (extrinsic) in an atopic person. A person suffering from atopy has a personal history of symptoms from nose, lungs and skin with hay fever (allergic rhinitis), eczema or urticaria often from childhood (childhood asthma). Common allergens are the house-dust mite or its faeces, pollen grains, moulds and domestic pets. When a middle-aged non-atopic person develops asthma, an allergen is seldom identified. The condition is sometimes called intrinsic asthma. Within minutes from inhalation of an allergen there is an immediate, anaphylactic reaction (Fig. 33-5). Eosinophils recognise the allergen and release allergen specific IgE antibodies. The allergen-IgE complex is bound to IgE-receptors on the surface of granule containing mast cells, eosinophils and basophils. Hereby, mediators of anaphylactic reactions are released from the mast cell granules: Leukotrienes (= SRS-A) are strong bronchoconstrictors and also cause mucosal inflammation with oedema and hypersecretion. Prostaglandin D2 is also contributing with bronchoconstriction and vasodilatation with increased capillary permeability. Eosinophils release leukotrienes C4, PAF, major basic protein and eosinophilic cation protein, all of which are toxic to epithelial cells. Histamine is a powerful vasodilatator and may play some role for the hypersecretion and bronchoconstriction in asthma, but antihistamins have no effect. During an attack of asthma the bronchial wall is suffering (Fig. 13-8). The hypertrophic smooth muscles contract, capillary leak of plasma water results in oedema of the lamina propria, and hypersecretion of the mucous glands produces thick mucous, which the cilia can hardly move. All of this causes universal narrowing of the airways or occlusion by mucous. The airflow limitation results in wheezing respiration, and the patient feels dyspnoa. The attacks usually occur during the night often with coughs. Stethoscopy of the lungs reveals wheezing. A severe asthmatic attack may continue for hours and days, in which case the condition is called status asthmaticus. There is tachycardia and sometimes pulsus paradoxus (the pulse disappears due to a marked fall in both systolic and pressure amplitude during inspiration). Some asthma patients develop a relative insensitivity of the adrenergic b2-receptors of the bronchial smooth muscles (down-regulation of the b2-receptors). All b-receptors act through activation of adenylcyclase and cAMP. When noradrenaline binds to b2- receptors it causes bronchodilatation, but not always sufficient in asthma. b2-adrenergic agonists interact with the bronchodilatating b2-receptors, but they also cause tachycardia by stimulating the b1-receptors of the myocardium. The b2-receptor agonists (salbutamol or terbutaline aerosols) are effective in mild asthma. - Cardioselective adrenergic b1-blockers must be administered with care to patients with a combination of asthma and cardiac disease. Anticholinergic bronchodilatators bind to muscarinic M1 and M3 receptors of the airways, and selective muscarinic antagonists such as ipratropium or oxitropium by aerosol are used as supplement to salbutamol. Previously, atropine - a non-selective muscarinic antagonist - was used. These drugs are rather ineffective in asthma. Anti-inflammatory drugs (Na+ -cromoglycate, nedocromil- Na+) blocks a chloride channel in the inflammatory cells, thus preventing Ca2+ influx, and thereby liberation of mediators. They are given to cases of mild asthma (children) before stimulation such as exercise. Corticosteroids (beclomethasone dipropionate or fluticasone propionate) are administered by inhalation, and they are effective in severe cases. The activation of inflammatory cells is rapidly decreased by local corticosteroids, which have minor systemic side effects only. A2. Chronic bronchitis & emphysema Chronic obstructive bronchitis is an inflammation of the bronchioles characterised by excessive production of mucous from hypertrophic mucous glands. There is an increase in the number of gel secreting goblet cells (Fig 13-7). The lumen contains large amounts of mucus and pus. The ciliated columnar epithelium is ulcerated and sometimes replaced by squamous cells without cilia (metaplasia). The small airways are narrowed, and their walls thickened by inflammation and oedema. There is morning cough with sputum for at least 3 months of the year for at least two years (WHO). This is a clinical diagnosis based on the patient history. Emphysema is an patho-anatomical diagnosis characterised by enlargement of the air spaces and destruction of the lung tissue distal to the terminal bronchiole (a tissue unit called an acinus or a primary lobule). The emphysematous lung has increased compliance (increased dV/dP) because the elasticity is decreased. Destruction of the alveolar walls includes the capillary bed with increased pulmonary vascular resistance causing pulmonary hypertension. Emphysema is established at autopsy. The most common type of emphysema is centri-lobular emphysema, where the damage is limited to the central part of the lobule or acinus, whereas the peripheral alveolar ducts and alveoli are preserved. The rare type of emphysema is called pan-lobular or pan-acinar, because the entire lobule is destroyed. - Bullous emphysema is when the entire lung consists of large cysts or bullae with hardly any normal tissue left. Chronic bronchitis & emphysema is synonymous with many alternative terms: Chronic Obstructive Airway/Lung/Pulmonary Disease or abbreviated COAD/COLD/COPD. Both bronchitis and emphysema co-exist in many patients. Some of these patients are dominated by the first, others by the second, and some have elements of asthma too. These disorders are almost exclusively confined to smokers (cigarette smokers in particular), and the severity of the disease is proportional to the amount of tobacco (number of cigarettes) smoked per day. The disorders are progressive during years of smoking and cause impaired exercise capacity. A patient smoking more than 25 cigarettes per day have a mortality that is 20 times higher than that of a non-smoker. Other airway irritants such as atmospheric pollution contributes to the death rate. The maintained irritation of the epithelium from smoke causes the hypertrophy and the hypersecretion of the mucous glands in the larger airways (Fig. 13-7). Surfactant normally lowers the surface tension of the alveolar fluid layer, but smoke has an adverse effect on surfactant. A high frequency of acute airway infections increases the pulmonary damage. The small airways of smokers are infiltrated with neutrophils, which are also present in their lumen. Neutrophils release elastase and proteases. These enzymes destroy lung tissue and produce emphysema, when not balanced by antienzymes such as antiproteases. A typical antiprotease in normal serum is hepatic a1-antitrypsin, which is inactivated by smoking. The main phenotypes of the a1-antitrypsin gene are MM= normal, MZ= heterozygous deficiency, and ZZ= homozygous deficiency. Hereditary deficiency only accounts for a minor part of emphysema. In the population with the susceptible phenotypes (MZ and ZZ), smokers develop emphysema 20 years sooner than non-smokers. Smokers with the phenotype PiZ are at a high risk of developing emphysema. The patient complains of smoker’s cough with large morning expectoration (ie, large quantities of sputum - purulent during exacerbation). Fog and pollution worsen the condition. As the lung function deteriorates, breathlessness (dyspnoea) becomes so severe that even dressing or tooth brushing feels like heavy exercise. The patient expires for a long time and with a snapping inspiration. The intercostal space is drawn in under inspiration and the accessory respiratory muscles are active. The lungs are hyperinflated and extend between the heart and the chest wall. Some patients are thin “pink puffers” or “type A emphysematous fighters”. Despite their severe dyspnoea, their arterial blood gasses are close to normal (point i in Fig. 14-7). They are often emphysematous with over-expanded lungs but with little bronchitis. As the term implies these patients are not cyanosed. Other patients are overweight “blue bloaters” or “type B bronchitis non-fighters”, because they seem to have given up the tiring respiratory effort at the expense of hypoxia and cyanosis. They often have symptoms of bronchitis and suffer from coughing, hypoxaemia, secondary polycythaemia, cor pulmonale (see below), and carbon dioxide retention with respiratory acidosis (Ch 17). These patients are typically cyanosed, and they suffer predominantly from chronic bronchitis - maybe with little centriacinar emphysema. The patients show little respiratory effort, which explains why they become cyanotic. Cor pulmonale, with body fluid retention (increased extracellular fluid volume), is demonstrated by a raised jugular venous pressure and ankle oedema. The hypercapnia (see below) results in peripheral vasodilatation, tremor, confusion, coma, and papiloedema. The two clinical pictures are seldom clean and often overlap. Many COLD patients are thin – typically the fighters - perhaps due to the high oxygen cost of breathing (often 30% of their oxygen uptake at rest), even food intake is a demanding task, and they tend to develop wasting. Obstruction of the airflow causes uneven ventilation; destruction of lung tissue reduces the capillary blood volume. The maldistribution of bloodflow upsets the normal matching of ventilation and perfusion (Ch. 14). This is the major cause of hypoxia and later hypercapnia. Hypercapnia signals alveolar hyperventilation. Half of all patients with severe breathlessness die within 5 years from hypoxia. Bronchodilatators, such as the b-adrenergic agonist salbutamol, may reduce the dyspnoea of many patients. Inhaled corticosteroids are marginally beneficial, but with only a few systemic side effects. Long term treatment with antibiotics is controversial, and most double blind controlled clinical trials show no effect. Mucolytics are ineffective for patients with COLD. Influenza vaccines are recommended for these patients as in other individuals at increased risk. The terminal stage is respiratory failure, which is characterised by hypoxia (ie, PaO2 of less than 7.3 kPa or 55 mmHg) and by hypercapnia (PaCO2 of more than 6.4 kPa or 48 mmHg) and severe disability. The hypercapnic patient has sacrificed a normal (Table 14-1) PaCO2, because it is much too costly for him in terms of energy expenditure for breathing. The patient is a blue bloater in a state of deep hypoxia with extremely low PaO2 and malnutrition. As the hypoxia persists the pulmonary arterioles constrict, which lead to pulmonary hypertension and cor pulmonale. Cor pulmonale is a heart condition secondary to pulmonary disorder with loss of pulmonary vessels and increased pulmonary resistance (Chapter 14). The lung disease causes pulmonary hypertension, increased work load of the right heart, right ventricular hypertrophy, and finally right heart failure. Fig. 13-9: Upper airways of a healthy person and of a patient with obesity and obstructive sleep apnoea. This patient also suffers from the Pickwick syndrome. - The airway pressures are given in kPa. Patients with chronic bronchitis and emphysema – among others - may complain of sleep apnoea. The normal short periods of apnoea occurring during REM sleep are prolonged, the patient wakes up in fear of suffocation, and snoring is frequent. The upper airways are obstructed in the supine position (Fig. 13-9) and the patient may develop severe hypoxia. Obstruction of the pharynx causes an abnormally high negative pressure in the airways (Fig. 13-9, below). During daytime the patient complains of headache and somnolence. Some of these patients are extremely overweight and develop a restrictive lung disorder due to accumulation of fat in the mediastinum and abdomen (Fig. 13-8). They suffer from frequent periods of somnolence and cyanosis during daytime due to hypoventilation, and they exhibit secondary polycythaemia and low PAO2 (the Pickwick syndrome). Cystic fibrosis is an autosomal recessive inherited disease of all exocrine glands, caused by a gene mutation on chromosome 7. A specific error results in a defective transmembrane regulator protein (the cystic fibrosis transmembrane conductance regulator). This is an a-adrenergic gated chloride channel. Normally, an elevated cAMP in the epithelial cell will open the chloride channel. In cystic fibrosis this does not happen, and with less excretion of NaCl to the airways, sweat ducts and pancreatic ducts, there is less excretion of water and thus increased viscosity of the secretions. Viscous secretions plug the airways and duct systems. New-borns with recurrent bronchopulmonary infections must be suspected of cystic fibrosis until disproved. It is too late to await airflow limitations. The diagnosis is confirmed by three sweat tests with a NaCl concentration above 60 mM. Patients with cystic fibrosis not only suffer from pulmonary infection with obstructive lung disease, bronchiolitis and bronchiectasis, but also from pancreatic insufficiency. Therapy is improved by administration of ATP, which stimulates nucleide receptors independent of cAMP. Hereby, the Cl- excretion is stimulated. Low lung volumes, measured as reduced total lung capacity (TLC) and vital capacity (VC), characterise restrictive lung diseases. Restrictive lung disease with small lung volumes (VC) is shown in Fig. 13-6. Also the TLC is small, and all volumes are often proportionally decreased. The airflow velocity and relative forced expiratory volume in 1 s is typically normal. One way or the other, the normal expansion of the lungs is restricted or the pulmonary compliance is decreased. The restrictive disorders are divided into those localised in the B1. lung parenchyma, and B2. chest wall including its neuromuscular apparatus and the pleura. In newborns there is a third restrictive disorder: B3. The respiratory distress syndrome. B1. Restrictive disorders of the lung These disorders comprise granulomatous disorders, systemic connective tissue disorders, extrinsic allergic alveolitis, diffuse pulmonary fibrosis, collapsed alveoli (atelectasis) and alveolar oedema. Granulomatous disorders are characterised by granulomas, which are nodules of inflammatory cells (macrophages, histiocytes, T-lymphocytes, and multinucleated giant cells) that are reacting to an irritant. The irritant is derived from micro-organisms (tubercle bacilli, fungi etc.), helminths, neoplasm or hypersensitive cells. There is a decrease in the number of circulating T-lymphocytes, because they are concealed in the lung tissue and the hilar lymph nodes. Restriction is often combined with obstruction. Sarcoidosis is a restrictive, granulomatous disorder characterised by bilateral hilar lympadenopathy with pulmonary infiltration and fibrosis on chest X-ray. In some cases there are skin sarcoidosis in the form of erythema nodosum (painful red nodules on the shins), inflammation of the uvea (uveitis), parotitis, acute arthritis or fatal involvement of the CNS. Systemic connective tissue disorders such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and systemic scleroses (generalized scleroderma) are sometimes complicated by interstitial lung fibrosis with restrictive disease. In RA there is pulmonary effusion with adhesions and restriction of thoracic expansion. In SLE, with plasma antibodies against nuclear components, there is recurrent pleurisy with pleural exudates and restricted breathing. In systemic sclerosis there is interstitial fibrosis occurring as widespread cysts called the honeycomb lung. The honeycomb lung is a term used for a typical radiological picture of small, thick-walled lung cysts (dilatated lung lobules). Extrinsic allergic alveolitis is caused by inhalation of many types of organic dusts containing antigens. Heavy occupational exposure results in a type 3-hypersensitivity pneumonitis (Chapter 33). Three examples are described here. Farmer’s lung is due to inhalation of the spores of thermophilic actinomycetes and micropolyspora faeni. Maltworkers lung is due to inhalation to the spores of aspergillus clavatus, when turning germinating barley. Bird fanciers lung is due to antigens present in feathers and in avian excreta. - Many different drugs and also radiation may cause pulmonary tissue reactions, with or without allergy, with interstitial fibrosis, alveolitis and restrictive disease. Diffuse interstitial pulmonary fibrosis is the terminal stage of many lung disorders, which may end up as a honeycomb lung (see above). The characteristic pathology is the thick alveolar interstitium all over the lung (Fig. 13-8). The serious condition is emphasised by the fact that the arterial blood gas tensions are low. The patient is dyspnoeic at rest, and the degree of hypoxaemia is explained by the ventilation-perfusion-inequality. The pulmonary diffusing capacity for oxygen is often reduced by 75% compared to normal (Ch 15). Pulmonary compliance is reduced, when alveoli collapse (atelectasis) or when left heart failure causes alveolar oedema (Fig. 10-10). B.2. Restrictive disorders of the chest wall These disorders comprise rib fractures, damage of the trachea or major bronchi, kyphoscoliosis (hunchback), ankylosing spondylitis, pneumothorax, pleural effusion, and neuromuscular disorders (poliomyelitis, myasthenia gravis, Guillain-Barre syndrome etc). Rib fractures are mainly caused by trauma, but they can also occur as the consequence of metastases or osteoporosis. Rib fractures are painful and the pain prevents sufficient ventilation and coughing. Traffic accidents may produce so many rib fractures that a flail segment moves inward during inspiration (flail chest). Such paradoxical movements cannot ventilate the underlying lung tissue sufficiently. Kyphoscoliosis should be corrected as early as possible, because later the restrictive ventilatory condition develops into hypoxaemia due to ventilation/perfusion inequality. Finally hypercapnia ensues, and the patient die from respiratory failure or pneumonia. Ankylosing spondylitis present itself as back pain with morning stiffness. The disease is genetic with a high frequency among B27-positive subjects (HLA-B27). Thoracic movements are reduced due to fixation of the vertebral joints and the ribs. Low lung volumes and chest wall compliance is combined with normal airway resistance. Pneumothorax means that air has entered the pleural space from the lung, or pneumothorax is due to a chest wall trauma. Normally, the pressure in the pleural space is subatmospheric, because the elastic recoil forces of the lung and chest wall drag in opposite directions. Communication with the atmosphere eliminates the pressure difference, the lung collapses and the thorax expands. Spontaneous pneumothorax means that pleura is suddenly ruptured without known cause. The rupture typically occurs apically, where the mechanical tension is largest due to expansion. The sudden pain is pleuritic (accentuated by inspiration or coughing), there is dyspnoea, no breath sounds by auscultation, and drum sounds by percussion of the affected area. Chest X-ray (Fig. 13-10) confirms the diagnosis. Once the leak has closed, air will be reabsorbed, because the total sum of partial pressures of the gases in the passing blood is lower than the atmospheric pressure prevailing in the pleural space or cavity (Krogh´s sliding equilibrium). Fig. 13-10: Drawing of the characteristic X-ray findings in a large spontaneous (left) and a case of tension (right) pneumothorax. Tension pneumothorax is, fortunately, quite rare - but an emergency. When air can be sucked into the pleural cavity through the rupture during inspiration, and cannot escape during expiration, the pneumothorax enlarges from breath to breath. The condition arises when the rupture functions as a one-way-valve. Signs of mediastinal shift are tracheal deviation and movement of the heart towards the other side on the chest X-ray. The large veins and heart becomes progressively compressed and the venous return to the heart suffers (Fig. 13-10). The incomplete diastolic filling leads to imminent cardiac failure and death may occur suddenly. Intervention must be rapid and primarily consists of establishing an open pneumothorax until tube drainage with underwater seal can be established. Pleural effusion is defined as accumulation of liquid (fluid except air) in the pleural space. Chest movements are reduced, breath sounds are absent, and percussion is dull. The X-ray confirms the diagnosis. Analysis of pleural fluid allows distinction between an exudate, transudate or pus. Transudates have a low content of proteins including lactic dehydrogenase. Transudates are pleural fluids that complicate hypoproteinaemia of any cause (hunger-oedema, nephrotic syndrome and heart failure). Exudates are pathological pleural fluids caused by malignant tumours (bronchial carcinoma, mesothelioma) or by malignant inflammations (tuberculosis, pulmonary infarction), and exudates are often bloodstained. Haemo- and chylo-thorax describe the accumulation of blood and lymph in the pleural space, respectively. Poliomyelitis, postinfective polyneuropathy (Guillain-Barré), myasthenia gravis and other neuropathies can affect the nerve supply to the respiratory muscles (the most important is the diaphragm) and cause restrictive lung disease with sleep apnoea and respiratory failure. B3. The Respiratory Distress Syndrome of newborns Respiratory distress in premature infants is caused by inadequate synthesis of surfactant by the type 2 cells. Such infants have lungs with enormous surface tension forces and low compliance, causing collapse of alveoli (atelectasis) and oedema (Fig. 10-10). Positive-pressure ventilation opposes these changes and may improve gas exchange. Administration of aerosolised surfactant is effective. · The law of ideal gasses. The ideal gas equation reads: Eq. 13-1: P×V = n×R×T. One mol of gas occupies a volume of 22.4 l at Standard Temperature (273 K), Pressure (one atmosphere = 101.3 kPa = 760 mmHg), Dry air (STPD). - The fact that the product of the pressure and volume of a fixed mass of gas is constant at constant temperature was discovered by Robert Boyle in 1660 (Boyles law). If the temperatures are the same in two states of one mass of gas, then: Eq. 13-2: (Boyles law): P1 × V1 = P2× V2 = constant. Boyle’s law (Boyle-Mariottes law) is not a fundamental law like Newton’s laws or the law of conservation of energy, but a practical approximation for real gas. · Poiseuille’s law. The driving pressure (DP) for laminar airflow (V°E) through the airway resistance is the intrapulmonary pressure (Palv) minus the external barometric pressure, PB. Poiseuille’s law for laminar air flow is an analogy to Ohm’s law: Eq. 13-3: Raw = DP/ V°E. Airway resistance (Raw ) is directly related to the air viscosity (h) and to the length (L) of the tube, and inversely related to its radius in the 4th power: Raw = 8 h L/r4. Doubling the length of the airways only doubles the airway resistance, but halving the radius increases the resistance sixteen-fold. · The law of Laplace: For a thin-walled organ with two main radii, Laplace assumed that the transmural (internal) pressure at equilibrium was identical with the fibre tension in the wall (T) divided by the two main radii. For a spherical organ (bubble) such as the alveoli, the two radii are the same, which simplifies the equation Eq. 13-4: Transmural pressure = T/(2r), where T is the total wall tension (elastic recoil plus surface tension; N per m) and r is the radius. · Rohrers equation. Laminar or streamline flow (the streamlines move parallel to the sides of the tubes) is limited to airways with low airflow velocities and smooth walls. Such conditions are normally present in small airways. Laminar flow is silent. However, all airways branch and there is transitional flow at each bifurcation. This transitional (laminar-turbulent) flow depends on the following driving pressure: Eq. 13-5: DP = [V°E × R1 + V°E2× R2]. The R-symbols denote constants. The second (turbulent) component is small during quiet breathing. · Bernoulli’s equation states that the total driving energy, applied to a continuously flowing ideal fluid volume (dV flowing frictionlessly and laminarly), equals the sum of 3 types of energy: the kinetic energy (1/2 r v2 - fluid density multiplied by the squared velocity) , the potential energy at the height (h) and the gravity (G), and the laterally directed energy (the lateral pressure, P, directed towards the walls). Eq. 13-6: Total energy = dV (1/2 r*v2 + h*r *G + P). The lateral pressure is highest where the velocity is lowest. The equation of continuity states that the velocity varies inversely with the cross-sectional area of the tube. Consequently, the lateral pressure is highest where the cross sectional area of the tube is largest. This is surprising as it may seem. · Reynolds equation for turbulent flow (eg, energy demanding whirls or eddy currents in a fluid) states that the critical, volumetric mean velocity (v) is directly proportional to the viscosity of the fluid (h), Reynolds-number (Rey), and inversely proportional to the density (r ) and the radius, r: Eq. 13-7: v = h*Rey/(r*r ). Turbulence is audible. The viscosity (h) of body-warm air (in the airways) and of blood is 1.88*10-2 and 4 mPa*s, respectively. The density (r ) of body-warm air (saturated with water vapour) and of blood is 1.15 and 103 kg m-3, respectively. The critical Reynolds number is 1200 for most fluids including body-warm air and blood. · The three lung volume conditions are derived from the law of ideal gasses. Consider a cylinder with a movable piston containing n moles of a gas at volume, V, at a certain pressure and temperature. At the above described standard conditions (STPD) the following equation applies: VSTPD×760/273 = n×R. Consider the same mass of gas at room temperature (t oC or 273+t K), saturated with water vapour, and at actual barometric pressure (PB). These conditions are known as ATPS (Ambient Temperature, Pressure, and Saturated with water vapour at tension Pwater). The air volume rises with temperature: VATPS×(PB-Pwater)/(273+t) = n×R. Now consider the same amount of gas at the conditions present in the alveoli; the air is saturated with water vapour, which exerts a partial pressure of 6.3 kPa (47 mmHg) at 37 oC, at ambient pressure. These conditions are known as BTPS (Body Temperature, ambient Pressure, and Saturated with water vapour). At BTPS conditions the air volume only varies with barometric pressure: VBTPS×(PB-47)/(273+37) = n×R. Since we have considered one mass of gas the products of volume and pressure divided by temperature, must in all three states equal n×R. This is expressed in the following three equations, the constants being those applicable with pressures in kPa: Eq. 13-8: VSTPD×101.3/273 = VATPS×(PB-Pwater)/(273+t) = VBTPS×(PB- 6.3)/(273+37) = n×R. A real gas has a finite size of the molecules, which reduces the effective volume of the space. The real (actual) gas pressure is smaller than the ideal, because of attractive intermolecular forces. Real gasses do not obey the ideal gas equation (Eq. 13-1). However, the deviations from the ideal gas law are acceptable at the pressure (P) and temperatures (T) of life on earth. I. Each of the following five statements have True/False options: A. The lateral pressure is highest where the cross sectional area of a tube is smallest. B. Emphysema is destruction of lung tissue distal to the terminal bronchioles. C. Clearance of the respiratory bronchioles is typically accomplished within an hour. D. Asthma is an acute obstructive lung disease, with reduced lumen due solely to bronchoconstriction. E. Reduced airway resistance characterises obstructive lung disease. II. Each of the following five statements have True/False options:
A 24-year-old male, with an oxygen uptake of 333 ml STPD/min, is breathing from a metabolic ratemeter containing 50 l of atmospheric air with an oxygen fraction of 0.2093. The room temperature is 293 K, the water vapour tension is 18 and PB is 760 mmHg.
A male with a FRC of 2.5 l shows an intrathoracic pressure change of 3 cm of water during normal tidal breathing of 0.5 l. His chest wall compliance is 0.15 l BTPS per cm of water. He has a total alveolar wall tension force (T) of 0.07 N/m tending to collapse two alveoli with radius 0.00004 and 0.00008 m, respectively. The total alveolar wall tension consists of the surface tension plus the elastic recoil forces. 1. Calculate the DP, which can prevent collapse of the two alveoli. 2. Is this result consequential for the stability of his alveolar design? 3. Is there a natural solution to this problem? 4. Calculate the specific lung compliance of this patient and compare it to the normal value. 5. What pressure must be applied to supply this person with one l (BTPS) of air per breath under positive-pressure ventilation. Try to solve the problems before looking up the answers. · Air passes into the airways through the nose and mouth, where it is warmed, humidified and filtered. From the trachea to the alveoli, there are 23 generations of airways. The first 16 (as an average) constitute the conducting zone, which is an anatomic dead space, because no gas exchange takes place. The 17-23 generations are the respiratory zone. · The lung-thoracic wall system consists of two elastic components that work together: the lungs, which behave like a balloon trying to collapse, and the thoracic cage trying to expand. · The barometric pressure (PB) is one atmosphere and is frequently defined as a zero reference point. All pressures measured are given in reference to the barometric pressure, which is the pressure at the mouth or at the surface of the thoracic cage. · The lateral pressure is highest where the cross sectional area of the tube is largest. · Dynamic airway compression: The lateral pressure is lowest where the cross sectional area of the tube is smallest and the velocity largest (Bernoulli’s law). The external pressure exceeds the lateral pressure and the airway is compressed. · Coughing causes momentary collapse of the tracheal wall. · Turbulent flow is audible. · Normal lungs are very distensible at functional residual capacity (FRC), but stiffen progressively towards total lung capacity (TLC). Lung distensibility is called compliance. · Compliance is an index of expandability of elastic organs and defined as the change in volume per unit change in pressure (dV/dP). The falling compliance during inflation near TLC is caused by an increase in the air-liquid surface tension, because the liquid contains tension-reducing molecules (surfactant) that are spread further and further. · The lungs and chest wall move together and support each other. This is what makes the total standard compliance of the respiratory system less than that of the lungs or rib cage alone. · Two forces are opposing lung expansion: The overall- elastic recoil of the lung, and the non-elastic or airflow resistance. · Surfactant is a complex phospholipid that is a combination of dipalmitoyl phosphatidylcholine (DPPC) and other lipids and proteins. DPPC orients perpendicular to the air-water interface, such that the charged choline base is dissolved in water (hydrophilic) and the nonpolar, hydrophobic fatty acids projects toward the alveolar air. The type 2 alveolar epithelial cells secrete surfactant. · Surfactant lowers the surface tension importantly in the alveoli, thereby increasing the lung compliance. · b2-adrenergic agonists interact with the bronchodilatating b2-receptors, but they also cause tachycardia by stimulating the b1-receptors of the myocardium. · Respiratory distress syndrome in premature infants is caused by inadequate synthesis of surfactant by the type 2 cells. Such infants have lungs with enormous surface tension forces (low compliance), causing atelectasis (collapse of alveoli) and oedema. · Chronic bronchitis is characterised pathologically by hypertrophy of the mucous glands of the bronchi, in combination with an increase in the number of gel secreting goblet cells. The bronchial wall is oedematous and inflamed. · The most common type of emphysema is centri-lobular emphysema, where the damage is limited to the central part of the lobule or acinus, whereas the peripheral alveolar ducts and alveoli are preserved. The glossary Committee of the International Union of Physiological Sciences (IUPS): “Glossary on respiration and gas exchange”. J. Appl. Physiol. 35: 941-961, 1973. Rahn, H., A.B. Otis, L.E. Chadwick, W.O. Fenn. The pressure-volume diagram of the thorax and lung. Amer. J. Physiol. 146: 161-166, 1946. Katzung BG. Basic & Clinical Pharmacology. 11th Ed. Appleton & Lange, Stanford, Connecticut, 2007.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
Click here to introduce your comments or contributions