New Human Physiology | Paulev-Zubieta 2nd Edition
Chapter 33: Infectious Diseases
| HOME | PREFACE | TABLE OF CONTENTS | SYMBOLS | SECTION INFO | CONTRIBUTORS | LINKS | CONTACT US |
Highlights
Study_ObjectivesPrinciplesDefinitionsEssentials
PathophysiologyEquationsSelf-AssessmentAnswers
Further Reading
|
Chapter 33
|
 |
|
|
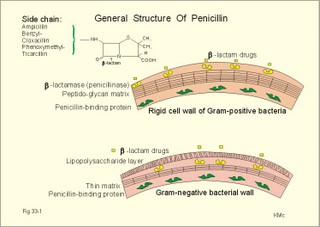
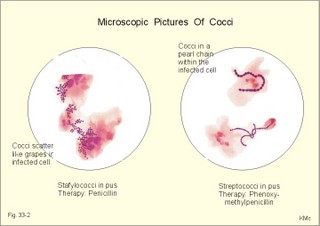
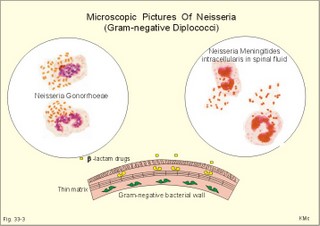
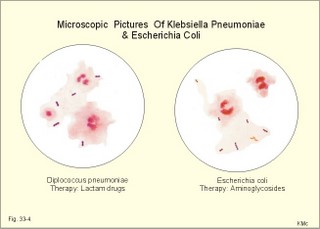
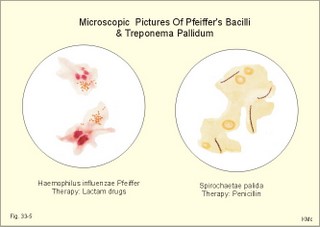
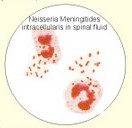
· To define bacteraemia, bactericidal antibiotics, bacteriostatic drugs, inflammation, infection, active and passive immunity, opportunistic infections, parasitism, pyaemia, septicaemia, symbiosis, and viruses. · To describe the effects of aminoglycosides, b-lactam drugs chloramphenicol, erythromycin, nitroimidazol, quinolones, sulphonamides, and tetracycline. · To explain well-known infectious disorders caused by bacteria, virus, fungi, protozoan, and helminths. · To use the concepts in problem solving and case histories. · Both unicellular microorganisms and multicellular organisms can live within the human body with beneficial (symbiosis) or detrimental (parasitism) consequences. · Febrile infectious diseases increase sympathetic nervous activity and raise the heart rate by release of nor-adrenaline. · Aminoglycosides are compounds of amino sugars derived from Streptomyces. Streptomycin is seldomly used due to oto-and nephrotoxicity. Neumycin is used for local infections. Gentamicin and tobramycin are bactericidal for many Gram-negative microbes. Netilmicin and amikacin are resistant to aminoglycoside-inactivating enzymes. · b--lactam drugs: The general structures of penicillin and cephalosporins include a b-lactam square. Lactam is a cyclic amide, and here the amine group is located on the second carbon from the carbonyl. · Bacteraemia refers to the presence of bacteria in the blood. · Bactericidal drugs possess the capacity to kill microbes. · Bacteriostatic drugs prevent the growth of microbes. · Chloramphenicol is a nitrobenzene-containing antibiotic used for the treatment of plague (Yersinia pestis) and enteric fevers (Salmonella typhi murium, Salmonella paratyphi). The most serious toxic effect of chloramphenicol is irreversible bone marrow depression. · Erythromycin and other macrolides (azithromycin, clarithromycin) are used against infections with Bordetella pertussis (whooping cough), Campylobacter, Clamydia, Coxiella, Legionella, Listeria, Mycoplasma and Toxoplasma gondii. Macrolides bind to and prevent translocation on bacterial ribosomes but not on mammalian ribosomes. · HIV means Human Immuno-deficiency Virus · Immunity. Active immunity is achieved by disease or by vaccination with live attenuated microbes, dead organisms or fractions of organisms, microbial toxins or antigen preparations produced by recombinant DNA technology. Childhood immunisation is maintained with booster doses throughout life. · Infections are diseases caused by microorganisms, viruses, protozoan and helminths. · Inflammation is the response of the body to damage or irritation. Inflammation is a vascular reaction, where leucocytes and fluid is transported from the blood into extravascular tissues. · Nitroimidazoles, such as metronidazole, inactivate anaerobic bacteria and certain protozoa by breaking up the DNA of the microbes. Indications are amoebiasis, giardiasis, trichomoniasis and anaerobic bacterial infections. · Macrolides are bactericidal antibiotics that bind to and prevent translocation on bacterial ribosomes but not on mammalian ribosomes. · Opportunistic infection refers to side-infection in immuno-deficient patients with TB, AIDS or other serious disorders. The most common opportunistic infection in AIDS is the pneumocystis carinii infection, which attacks the lungs. · Parasitism refers to a condition, where two dissimilar organisms live together to the benefit of the parasite and to the detriment of the host (protozoan and helminthic infections). · Prions (small proteins) and viroids (small nucleic acids) can live in humans and may contribute to human disease (Creutzfeld-Jacobs disease, dementia etc). · Pyaemia is septicaemia with emboli causing abscesses in the brain, lungs, liver or other sites in the body. · Quinolones inhibit bacterial DNA gyrase, which normally maintains the helical structure of DNA. These antibiotics are used for infections with resistant microbes. · Rickettsias are extremely small bacteria that are transferred to humans by rat fleas, human lice, mites and tics - often by scratching. They cause different types of Typhus fever. · Septicaemia refers to a condition, where microorganisms multiply in the blood, cause high fever, fall in blood pressure and shock. · Sulphonamides contain an essential para-amino group and inhibit folic acid synthesis in the microbes. These drugs are used for urinary tract infections and for inflammatory bowel disease · Symbiosis refers to a condition, where two dissimilar organisms co-operate in order to benefit or survive. · Tetracycline contains a four-ring structure and act by preventing attachment of tRNA to the mRMA-ribosomal complex. Tetracycline inhibits a wide spectrum of aerobic and anaerobic Gram-positive and Gram- negative bacteria, Clamydia, Mycoplasma and rickettsia. · Viruses are small infectious agents, which contain either DNA or RNA, and only survive intracellularly. The general structure is a nucleic acid core and an antigen protein shell that is specific for each virus. Viruses are the only a-cellular, proteinaceous agents known to infect humans. This paragraph deals with 1. Antimicrobial therapy, 2. Antiviral drugs, 3. Antifungal drugs, 4. Anti-protozoan therapy and 5. Antihelmintic drugs. Antimicrobial agents attack young, growing cells. An increasing number of microbes develop resistance for multiple drugs. The practical cause is an increasing use of antibiotics for minor infections and blind inappropriate therapy. Resistance to an antibiotic develops by mutation. Bacteria that can produce penicillinase are resistant to some of the penicillin molecules. Antibiotics have toxic effects, especially when used in overdose or in the presence of other disease such as hepatic or renal failure. Aminoglycosides are both oto- and nephrotoxic. Antibiotics can lead to secondary infections with fungi or with Clostridium difficile. Serious bacterial infections and infections in immunodeficient patients are commonly treated with bactericidal drugs (aminoglycosides, cephalosporins, and penicillin), although there is no evidence that these drugs are more effective than bacteriostatic drugs. Such serious infections (eg, endocarditis, meningitis, TB, septicaemia) are preferably treated with combinations of synergistic antibiotics. - On the other hand, penicillin inactivates aminoglycosides. b-Lactam drugs. The general structures of penicillin and cephalosporins include a b-lactam square. Lactam is a cyclic amide, and here the amine group is located on the second carbon from the carbonyl (Fig. 33-1). The small square has a low stability, and benzylpenicillin (penicillin G) undergoes hydrolysis rapidly by the acid gastric juice when given orally. Phenoxymethyl-penicillin (penicillin V) is more stable, and a sufficient fraction is absorbed following oral administration. Ampicillin is produced by introduction of an amino group into the phenyl radical of benzylpenicillin, which makes it active against both Gram-negative and Gram-positive bacteria. Further modification of the acyl side chain results in cloxacillin, which is insensitive to penicillinase, and thus preferable in treating infections with penicillinase- producing bacteria. The advantages of cephalosporins over penicillin are their resistance to penicillinase and their wider antimicrobial spectrum (both Gram-positive and Gram-negative bacteria). Fig. 33-1: Penicillin is build up by acyl side-chains linked to b-lactam and a thiazolidine ring. Cephalosporins have a dihydrothiazine ring instead. The b-lactam drugs interfere with bacterial cell wall development. Both gram-positive and gram-negative bacteria have a rigid cell wall composed of a matrix of peptidoglycan strands. Gram-positive bacteria do not have a lipopolysaccharide coat in contrast to the gram-negative bacteria (Fig. 33-1). The two groups of b-lactam antibiotics bind to and inactivate specific penicillin binding proteins. These molecules are peptidases involved in the final cross-link of the rigid peptidoglycan matrix. The b-lactam antibiotics block this final cross-linking reaction and thus the development of a normal bacterial cell wall. Bacteria that can produce b-lactamase (penicillinase) are resistant to several penicillins. Inhibitors of ribosomal actions. Aminoglycosides, chloramphenicol, clindamycin, erythromycin, fusidic acid, mupirocin, spectinomycin, tetracycline all bind to bacterial ribosomes and interfere with protein synthesis. Aminoglycosides are compounds of amino sugars derived from Streptomyces. Streptomycin is seldomly used due to oto-and nephrotoxicity. Neomycin is used for local infections. Gentamicin and tobramycin are bactericidal for many Gram-negative microbes. Netilmicin and amikacin are resistant to aminoglycoside-inactivating enzymes. Chloramphenicol is a nitrobenzene-containing antibiotic indicated for the treatment of plague (Yersinia pestis) and enteric fevers (Salmonella typhi murium, Salmonella paratyphi). Chloramphenicol binds to ribosomes, and prevents the addition of new amino acids to growing peptides. The most serious toxic effect of chloramphenicol is irreversible bone marrow depression. Erythromycin and other macrolides (azithromycin, clarithromycin) are used against infections with Bordetella pertussis (whooping cough), Campylobacter, Clamydia, Coxiella, Legionella, Listeria, Mycoplasma and Toxoplasma gondii. Macrolides bind to and prevent translocation on bacterial ribosomes but not on mammalian ribosomes. Fusidic acid has a bile acid structure and inhibits Gram-positive Cocci including penicillinase-producing Staphylococcus aureus in combination with other antibiotics. Fusidic acid inhibits translocation on the ribosomes and is hereby bactericidal for many bacteria. Tetracycline contains four-ring structure and act by preventing attachment of t-RNA to the bacterial mRMA-ribosomal complex. Tetracycline inhibits a wide spectrum of aerobic and anaerobic Gram-positive and Gram- negative bacteria, Clamydia, Mycoplasma and rickettsia. Nitroimidazoles. Nitroimidazoles, such as metronidazole, inactivate anaerobic bacteria and certain protozoa by breaking up the DNA of the microbes. Indications are amoebiasis, giardiasis, trichomoniasis and anaerobic bacterial infections. Quinolones (nalidixic acid, cinoxacin, and fluoro-based ciprofloxacin, lomefloxacin, ofloxacin, and norfloxacin) inhibit bacterial DNA gyrase, which normally maintains the helical structure of DNA. These antibiotics are used for infections with resistant microbes. Sulphonamides contain an essential para-amino group and inhibit folic acid synthesis in the microbes. These drugs are used for urinary tract infections and for inflammatory bowel disease. Idoxuridine and vidarabine are used as early as possible against herpes simplex virus and against varicella zoster virus (herpes zoster and severe varicella or chickenpox). Acyclovir inhibits viral DNA synthesis and is effective against the same virus disorders. Ribavirin is used against Lassa fever (see later). Azido-deoxy-thymidine inhibits HIV reverse transcriptase and thus impairs viral replication. This substance is used for HIV patients, although there is danger of bone marrow depression. Interferon is produced by the T-lymphocytes during virus infections. Interferon is used for hepatitis B and C. The target of antifungal drugs is young, growing cells. Polyenes such as Amphotericin B and nystatin bind to sterols in the fungal membranes and increase the permeability, so K+ and Mg2+ leaks out of the cell. Hereby, the fungi are killed. Mammalian membranes have a lower affinity for polyenes than fungal membranes containing ergosterol. Since amphotericin B is nephrotoxic, a combination therapy with flucytosine is used for serious systemic fungal infections. Flucytosine inhibits fungal DNA synthesis. Griseofulvin is used for long lasting fungal infections in skin and nails, because it is concentrated in keratin. Griseofulvin enters susceptible fungi and inhibits their mitosis. Imidazoles inhibit a membrane ATPase and incorporation of ergosterol in the cell membrane of susceptible fungi. This results in K+-efflux from the cell. Leishmaniasis is treated with meglumine antimoniate and Na-stibogluconate. These substances inhibit phosphofructokinase and Krebs cycle enzymes in the Leishmania organism. Malaria is caused by infection with the Plasmodium protozoa, which is present in the human host in the blood (erythrocytic) or the tissue (extra-erythrocytic stage). The erythrocytic stage is treated with aminoquinolines (eg, chloroquine) or analogues. Their antimalarial action is unclear, but they seem to be toxic to both the red cell and the plasmodia membranes. The extra-erythocytic stage is treated with primaquine. The diaminopyrimidines, pyrimethamine and trimethoprim, inhibit dihydrofolate reductase in malarial parasites. Diaminopyrimidines and sulphonamides act synergistic to prevent the formation of schizonts in erythrocytes and hepatocytes. African trypanosomiasis is treated with tryparsamide or melarsoprol. These arsenicals inhibit sulphydryl groups on carbohydrate enzymes in the parasite, whereby the production of ATP decreases. Chagas disease is caused by trypanosoma cruzi and treated with nifurtimox, which produces free radicals. The free radicals react with oxygen to form superoxide anion, hydroxyl-free radical, and hydrogen peroxide. The trypanosomes do not contain enzymes able to inactivate these reactive substances, so they cause peroxidation of lipids and ribonucleic acids (DNA, RNA) and the parasites dissapear from the tissues. Unfortunately, serious side effects occur at high doses (hemolytic anemia, neuritis and psychoses). The disease affects an estimated 16-18 millions of humans.Chagas disease is considered to be autoimmune with formation of autoantibodies against the second loop of the muscarine receptor (Dhein et al, 2001). Giardiasis and trichomoniasis are treated with quinacrine, which prevent parasite replication by interference with DNA. Helminths (worms) cause medical problems world-wide, because they are carried by parasitized humans all over. The helminths are divided into three groups: 5a. Roundworms (ie, nematodes), 5b. Flukes (ie, trematodes, flatworms), and 5c. Tapeworms (ie, cestodes, flatworms). The existence of the worm in the host depends on its movements in order to reach an optimal location for food, on glucose and other nutrients, and on intact cytoplasmic microtubules. 5a. Roundworm disorders are treated with mebendazole or with thiabendazole. These substances bind to the cytoplasmic microtubules of the roundworm and inhibit glucose transport and protein secretion. 5b. Flukes are sensitive to praziquantel, which attacks the surface barrier (tegumentum) and the muscles of the worm. Praziquantel destroys the surface of the worm so host antibodies can bind to the worm antigens. Hereby, host complement and leucocytes are attracted to the site and a large Ca2+-influx into the worm cells is triggered. The worm muscles enter a spastic contraction and the worm is killed by killer cells. 5c. Tapeworms are also killed by praziquantel, but as an alternative they are sensitive to niclosamide. Niclosamide binds to the mitochondria of both host and parasite and block ATP formation. Gut-dwelling tapeworms absorb niclosamide but not gut-dwelling roundworms. Therefore, tapeworms exposed to niclosamide cannot produce ATP, their muscles are ineffective, they loose their grip in the intestinal mucosa and they are expelled. This section deals with 1. Bacterial infections, 2. Viral infections, 3. Fungal infections, 4. Protozoan infections, and 5. Helminthic infections. Gram-positive Cocci, gram-negative cocci, gram-positive bacilli, gram-negative bacilli, actinomycetes, mycobacterium, spirochaetes, rickettsia, and Clamydia cause bacterial infections. 1A. Gram-positive cocci Gram-positive cocci include staphylococci and streptococci. Staphylococci present in the microscope like clusters or grapes (Fig. 33-2). Staphylococci are normally found on the surface of the skin and at all natural openings of the human body. Skin infections with Staphylococcus aureus include cellulitis, furuncles, carbuncles, impetigo and staphylococcal toxin scarlet fever. Typical is also parotitis and osteomyelitis. Lung and airway infections may result in abscesses also in the lung. Endocarditis and pericarditis are serious just as meningitis and brain abscesses. A special syndrome occurs in young females using high-absorbency polyacrylate tampons. There is rapidly developing fever, erythema, vomiting, diarrhoea, myalgia and shock (ie, toxic shock syndrome caused by staphylococcal toxin-1). Staphylococcal food poisoning is caused by heat-stable enterotoxin (A-E) from replicating staphylococci in manufactured food (cans, milk etc). There is diarrhoea and the patient vomits persistently. Staphylococci outside hospitals are usually penicillin sensitive, and penicillin is preferred for infections with these organisms. Staphylococcal infections acquired in hospitals are often penicillin resistant. Accordingly, the patient is treated with fusidic acid in synergy with other antibiotics. Fusidic acid inhibits translocation on the ribosomes and is hereby bactericidal for many bacteria. Staphylococcus aureus and other species resistant to aminoglycosides and also to all b-lactam drugs are now spread throughout the world. These infections are preferably treated with the lipophilic cell wall inhibitor, teichoplamin, and with quinolones Fig. 33-2: Staphylococci and streptococci in pus under the microscope. Streptococcal infectionsStreptococci are round Gram-positive bacteria often arranged like a pearl chain in the infected cells (Fig. 33-2). Streptococcus pyogenes (group A b-haemolytic streptococci) cause almost all human infections such as classical scarlet fever and erysipelas. Persons deprived of neutralizing antitoxin-antibodies to erythrogenic toxin develop classical scarlet fever, when infected with streptococci. Scarlet fever is usually a mild childhood disease with an incubation period of 2-4 days. Fever, headache and vomiting are typical clinical features. On the second day a rash occurs on the skin covered by a T-shirt. After 5 days of rash the skin desquamates. Typical is circumoral palor and strawberry tongue. Otitis media or even a retropharyngeal abscess complicates scarlet fever, which can be life threatening. Phenoxymethylpenicillin is given orally for 10 days or erythromycin in penicillin-allergic individuals. Group A streptococci causes erysipelas. Erysipelas is a skin infection with red swollen skin. Sepsis can be terminal, so immediate penicillin therapy is imperative. 1B. Gram-negative diplococci Gram-negative diplococci are unmoveable bacteria, also called Neisseria, N (detected in 1879 by Albert Neisser). Neisseria gonorrhoea and N. meningitides are pathogenic to humans, and N. catarrhalis is present in the nasopharynx of all healthy persons. The diplococci are formed like a coffee bean (Fig. 33-3). Fig. 33-3: Neisseria gonorrhoea (N.G.) and Neisseria meningitides. b-Lactam drugs (penicillins and cephalosporins) block the development of the normal meningococcal or gonococcal cell wall. Aminoglycosides bind to bacterial ribosomes and interfere with protein synthesis. Quinolones inhibit bacterial DNA gyrase. Gonorrhoea. The incubation period is usually less than a week. The Neisseria gonorrhoea has a special affinity towards the epithelium of the genital tract and other natural openings. Quite a few patients - especially females - experience no symptoms. Males develop urethritis with discharge and dysuria (painful urination). Complications in the males include infections of the epididymis, the testes or the prostate. Females are frequently infected in the endocervical channel, the vagina and in the rectum as proctitis just as homosexual males. Ascending infection in females leads to salpingitis and a high incidence of infertility. Arthritis is a late complication. Direct microscopy reveals the diagnosis, or culture of the fastidious bacteria on special media may be necessary. Uncomplicated cases are cured by 3 g of the amino-penicillin, amoxillin, with probenecid to delay the renal secretion. Patients with allergy or penicillin-resistant cocci require the quinolone, ciprofloxacin. The effects of antibiotics are shown in Fig. 33-3. The meningococcus reaches the blood through the naso-pharynx. The disease is either a sepsis with or without meningitis. Acute meningococcal sepsis, where death ensues within hours, sometimes occurs epidemically. Meningococci are found in the blood or CSF. Cephalosporins, such as cefotaxime, or benzylpenicillin are effective when given immediately on suspicion. Vaccination is recommendable when travelling. 1C.Gram-positive bacilli The most important infections are diphtheria, tetanus, botulism, gas gangrene, listeria, anthrax and pseudomembraneous colitis. Diphteria is caused by airborne spread of Corynebacterium diphteriae. This is a club-shaped bacillus, which produces Diphteria toxin when exposed to bacteriophag B. Diphteria toxin has two subunits. Subunit A is toxic and subunit B transfers A to toxin-receptors on peripheral nerves and on the myocardium. Following a week incubation there is nasal discharge with crusts around the nares. A white membrane of fibrin, cells and bacilli characterizes the tonsillar and pharyngeal infection. Typical is also the bull-neck of swollen lymph glands. Laryngeal infection is life threatening due to airway obstruction with dyspnoea and cyanosis. Later myocarditis and palatal paralysis occur, followed by paresthesia, cranial nerve palsies and eventually encephalitis. Rapid administration of antitoxin i.v. is the only specific therapy of the toxin effects. Penicillin is given in order to kill the corynebacteria. Active immunisation in childhood is important. Even a trivial wound contaminated with Clostridium tetani can kill the un-immunised victim within 24 hours.Tetanospasmin is an extremely potent neurotoxin. Muscle spasms occur in the masseter muscle (lockjaw or trismus) and in the mimic facial muscles (grinning expression or risus sardonicus). Light or noise triggers spasms. Spasms of the back muscles result in opisthotonus (ie, arching of the body by spasms of the neck and back muscles). Death ensues from laryngeal spasms with respiratory failure or from cardiac arrest. Human anti-tetanus immunoglobulins are given i.m. and penicillins given i.v. Clostridium botulinum spores are thermo-stable, proliferate and produce neurotoxins pathogenic to humans (A, B and E) in canned foods. Botulinus toxins are thermo-labile and the most potent neurotoxins known. They block the neuromuscular endplate effectively. Neurological symptoms and signs occur within 24 hours after ingestion of contaminated food. Laryngeal spasm, strabismus, generalized paralysis including respiratory paralysis occurs, and the mortality is up to 70% of all hospitalised patients. Guanidine hydrochloride reverses the neuromuscular blockade, and assisted ventilation is often necessary. Clostridium perfringens causes most case of gas gangrene, which occurs in lacerated wounds such as gun wounds. The muscle tissue is oedematous and slowly filled with gas, which is felt as crepitus. There is a tachycardia and the patient dies in shock or from renal or hepatic failure. Debridement and antibiotic combination therapy is imperative. See also hyperbaric oxygenation in Chapter 19. Listeria monocytogenes causes listeriosis with septicaemia, abortions and meningitis. Listeriosis is treated with ampicillin and Gentamicin. Bacillus anthracis is spread from infected animals to man. There are erythematous skin lesions, retrosternal pains, pleural effusions, haematemesis and bloody diarrhoea. Death is often caused by respiratory failure. Serious cases are treated with penicillin i.v. Clostridium difficile produces toxins A and B following termination of antibiotic therapy. There is diarrhoea, fever and abdominal pain. The diagnosis is confirmed by the presence of toxin in stool specimens. Suspected antibiotics are of course seponated. Metronidazole or vancomycin is used for 10-14 days. 1D. Gram-negative bacilli Brucellosis is caused by Brucella abortus Bang, Brucella militensis and Brucella Suis. These microbes are Gram-negative coccobacilli. Brucella is spread by intake of raw milk from infected cows and goats. In the body Brucella spread along the lymphatic system from where they reach the blood and finally the reticulo-endothelial system. The patient experiences oscillating fever, myalgia and lympadenopathy. Blood culture establishes the diagnosis. Tetracycline combined with rifampicillin for 6 weeks is effective. Bordetella infections include pertussis (Bordetella pertussis) and parapertussis (Bordetella parapertussis). Pertussis or whooping cough is spread by droplets and contagious. The first week is the catarrhal stage, where the patient feels as with a common cold with light fever, and coughing triggered by vagal signals. The paroxysmal stage is characterized by attacks of typical whooping cough - often just following change of thoracic position. A whoop is a prolonged, wheezing inspiration caused by airways obstructed with oedema and mucus. The cough attack terminates in vomiting and expectoration of a viscid mucus. The total white blood count is dominated by lymphocytes. Complications include atelectasis, pneumonia, facial cyanosis, herniation, conjunctival petechiae and nose bleeding. Parapertussis is milder. The diagnosis is confirmed by culture of nasopharyngeal swabs. Early administration of erythromycin is beneficial. Escherichia coli infections include travellers diarrhoea, children’s diarrhoea, and diarrhoea in developing countries in general. The coli bacterium is a large, unmoveable Gram-negative stick (Fig. 33- 4) first described by Escherich. Serious infectious cholera-like diseases and bloody diarrhoea are also seen. The quinolone, ciprofloxacin, is effective, and in severe cases the aminoglycoside, Gentamicin, is used. Fig. 33-4: Klebsiella pneumoniae and Eschericia coli are closely related. b-Lactam drugs (cephalosporins) block the development of the normal Klebsiella pneumoniae cell wall. Aminoglycosides bind to the ribosomes of coli bacteria and interfere with protein synthesis. Quinolones inhibit colic DNA gyrase and interfere with the normal helical structure of its DNA. Klebsiella pneumoniae (Friedlander) is a short, unmoveable Gram-negative stick (Fig. 33-4) causing institution-acquired pneumonia in immuno-deficient patients. Cephalosporins are required, but the mortality is high. The effects of antibiotics are shown in Fig. 33-4. Haemophilus influenzae infections include meningitis, pneumonia, otitis media, endocarditis, pericarditis and milder infections. The diagnosis is confirmed by culture of Haemophilus influenzae Pfeiffer, which is a Gram-negative aerobic bacillus (Fig. 33-5). Serious infections must be treated immediately with cephalosporins (oral cefaclor). Chloramphenicol therapy is dangerous due to granulocytopenia or agranulocytosis. Cholera. Cholera is a disease caused by an enterotoxin produced by the gram-negative bacillus, vibrio cholerae. If this bacillus is allowed to proliferate within the lumen of the small intestine, it causes profuse watery diarrhoea - up to 24 l per 24 hours - dehydration and circulatory shock. Fulminant cholera can kill the patient within a day. The cholera enterotoxin contains A and B subunits. Subunit A is an enzyme, which enters the enterocyte and irreversibly activates adenylcyclase, whereby a cascade of reactions is triggered. Subunit B links the enterotoxin to the brush borders of the enterocytes, so the effect is persistent. As cAMP is activated in the cell it activates an electrogenic chloride-channel in the brush border membrane. This causes an enormous secretion of NaCl and water into the lumen of the small intestine. Although the colonic lavage (reabsorption capacity) is normally extremely large (up to 4200 ml reabsorbed fluid per day), this is not enough to prevent the massive diarrhoea (ricewater stool). Acute dehydration with loss of base leads to metabolic acidosis and hypovolaemic shock. Therapy is immediate rehydration and tetracycline. Tetracycline acts by preventing attachment of t-RNA to the mRMA-ribosomal complex of the cholera bacillus. Fig. 33-5: Haemophilus influenzae (Pfeiffer) and Treponema pallidum. b-Lactam drugs (penicillins and cephalosporins) block the development of the normal cell wall of the Pfeiffer bacillus. Penicillin for syphilis interferes with spirochaetal cell wall development. Salmonellosis includes typhoid fever (Salmonella typhi), paratyphoid fever (Salmonella paratyphi), and enterocolitis (Salmonella enteritidis, Salmonella typhi-murium). Salmonellae proliferate in Peyers plaques of the small intestine, and finally reach the reticuloendothelial system via lymph and blood. The quinolone, ciprofloxacin, is used as the preferred treatment. Shigellosis or bacillary dysentery is caused by a series of Gram-negative bacilli. Dysentery is the name of severe bloody diarrhoea with mucus and cramping abdominal pain. Complications include dysentery-arthritis, widespread infections and life-threatening shock. Sulphonamides or the quinolone, ciprofloxacin, are used. Campylobacter infection also causes bloody diarrhoea. Quinolone treatment is a frequent choice. Helicobacter pylori grow and proliferate in the mucous layer of the gastric and duodenal epithelium. This Gram-negative microbe is involved in the pathogenesis of peptic ulcer disease. Clarithromycin is a macrolide that binds to and prevents translocation on Helicobacter pylori- ribosomes, which is an effective basic therapy of peptic ulcer. Yersinia infections include plague (Yersinia pestis), enterocolitis (Yersinia enterocolitica), and Yersinia pseudotuberculosis. Plague is spread from woodland rodents to domestic rats. The rat flee bites humans. Bubonic plague occurs suddenly with high fever and the patient is confuse and may seem drunk due to toxaemia. The inguinal lymph nodes rapidly develop lymph-adenopathy or buboes. Pneumonic plague is fulminant pneumonia with bloody sputum and cardiac failure. Petechiae and severe cyanosis with a terminal outcome is responsible for the name the Black Death. Septicaemia plague is dominated by septicaemic shock and death occurs in days. The diagnosis is confirmed by demonstration of the bacilli in blood, sputum or lymph node aspirate. Rapid administration of antibiotics in synergism-combination is essential (streptomycin, tetracycline etc). Entero-colitis or terminal ileitis caused by the Y. enterocolitica, and pseudotuberculosis (mesenteric lymphadenitis) is treated with tetracycline. Tularaemia (Tulare is a town in California) is caused by Francisella tularensis, and spread from animals (in particular rabbits and squirrels) to man through flies, ticks and mosquitoes. There is an ulcer with lympadenopathy and sometimes pneumonia or septicaemia. The diagnosis is confirmed with an agglutination test. The aminoglycoside, gentamicin, is effective. Legionnaire disease is caused by Legionella pneumophilia. The clinical picture is that of a severe pneumonia with coughing, fever, tachypnoea, cyanosis, confusion and diarrhoea. The diagnosis is confirmed by rapid antigen tests. Erythromycin and rifampicin (anti-mycobacterial drug that inhibits RNA synthesis and thus protein synthesis) are effective. Macrolides, such as erythromycin, bind to and prevent translocation on bacterial ribosomes but not on mammalian ribosomes. 1E. Actinomycetes are branching bacteria (Gram-positive) that cause slowly and insidious developing infections with a typically chronic pattern. Actinomycosis and nocardiosis are rare disorders localised in lymph nodes, lung tissue, and coecum. Surgery and penicillin, tetracycline or the sulphonamide, sulphadiazine, are used. 1F. Mycobacteria are aerobic bacilli that grow slowly. Mycobacterium tuberculosis is the cause of most cases of human tuberculosis. The primary infection includes the lungs, where granulomas are formed with caseation centrally. Although the primary granuloma heals there is often surviving tubercle bacilli in the granuloma, and later the bacilli spread locally and with the blood. The spread can attack all parts of the body - frequently bones and the kidneys. Daily intake of rifampicin 600 mg and isoniazid 300 mg for half a year is necessary in order to cure pulmonary tuberculosis. Mycobacterium leprae causes leprosy or Hansens disease. This mycobacterium can oxidise 3,4-dihydroxy-phenylalanine to measurable pigments. Tuberculoid leprosy is localised, because the patient has maintained his cell-mediated immunity. The hypopigmented patches on the skin are anaesthetic.Lepromatous leprosy is generalized because the patient has impaired cell-mediated immunity. The lesions affect the skin of the face, and limbs. Leprosy is treated with dapsone (a folate synthetase inhibitor) and clofazimine daily. Each month a dose of rifampicin is given. Rifampicin (rifampin) binds to the mycobacterial RNA polymerase (less to mammalian RNA polymerase), and inhibits initiation of RNA synthesis. Isoniazid is bactericidal to growing mycobacteria - possibly by blocking the synthesis of mycolic acid in the bacterial wall. 1G. Spirochaetes Spirochaetes include Treponema, Leptospira and Borrelia. Syphilis (Lues) is caused by Treponema pallidum, which is mobile spirochaetes (Fig. 33-5). Congenital syphilis is acquired transplacentally from mother to foetus and is apparent a few weeks after birth. The babies pass through three stages of the disease similar to those of the adults. Adult syphilis is acquired by intimate sexual contact. Primary syphilis: Three weeks after exposure to the spirochaetes there is a papule at the epithelial lesion. The papule ulcerates and develops into a painless chancre with swelling of the regional lymph glands. Secondary syphilis: Three months following the exposure the patient experiences fever, sore throat, lympadenopathy, rashes, condylomata and arthralgia. These symptoms and signs usually fade away over a few months without therapy. Tertiary syphilis: Gumma in the skin, cardiovascular and neural damage (neurosyphilis) is typical findings years after the primary lesion. A gumma is a granulomatous mass often found to expand intracranially, where the pressure rises and focal disorders occur (epilepsy or hemiplegia). The fluorescent treponema antibody absorption test is specific for treponema and remains positive for life. Tertiary syphilis, with demyelinisation of the dorsal roots of the spinal cord is known as tabes dorsalis. The syndrome includes lightening or knife-tap pain, ataxic gait, neuropathic joints, ptosis, optic atrophy, and Argyll-Robertson’s light-stiff pupil (Chapter 7). Early syphilis is treated with procaine penicillin in large daily doses for two weeks. Neurosyphilis is treated with parenteral penicillin with steroid cover for three weeks. Yaws, Bejel, and pinta are caused by other treponema strains, but they produce the same late stages as seen in syphilis and they are all treated with the long-acting procaine penicillin. Leptospirosis is caused by Leptospira interrogans ictero-haemorrhagiae. This disorder is also called Weil’s disease. Borrelia recurrentis causes relapsing fever. Borrelosis or Lyme disease (first described in the city Lime in Connecticut) is caused by Borrelia burgdorferi. The disease is transmitted by infected tics. Borrelosis produces the same three stages as seen in syphilis. The first stage occurs within a week with skin lesions. Cardiac or neurological findings and IgM antibodies in the blood plasma characterize the second stage after months. Arthritis and IgG antibodies in the blood or cerebrospinal fluid characterize the third stage after years. Prompt treatment with large doses of benzathine penicillin or tetracycline for weeks may shorten the duration. Later stages must be treated with intravenous cephalosporins. 1 H. rickettsia Rickettsias are extremely small bacteria that are transferred to humans by rat fleas, human lice, mites and tics - often by scratching. They cause different types of Typhus fever 1 I. Chlamydiae Chlamydiae are intracellular bacteria infecting one of five persons. Chlamydia trachomatis causes trachoma, which is a common cause of blindness that can be avoided by tetracycline therapy. Other strains cause genital infections including lymphogranuloma venereum. Chlamydia psittaci causes psittacosis or ornithosis, which is spread from infected birds. Chlamydia pneumoniae causes pneumonia, which is treated with tetracycline. Viruses are small infectious agents, which contain either DNA or RNA, and only survive intracellularly. The general structure is a nucleic acid core and an antigen protein shell that is specific for each virus. The DNA viruses comprise adenovirus (acute pharyngitis, laryngitis or croup, mesenteric lymphadenitis), herpes viruses (cytomegalovirus infection, herpes simplex, varicella-zoster, Epstein-Barr virus infection, roseola infantum), papova-viruses (genital warts, carcinoma of the cervix), parvo-virus (slapped-cheek disease or erythema infectiosum, arthropathy, chronic infectious anaemia), and pox virus (smallpox or variola). The RNA viruses comprise picorna-viruses (poliovirus, Coxsackievirus, Hepatitis A, Echovirus, Enterovirus and Rhinovirus with common cold), reoviruses (reo-and rota-virus causing childhood diarrhoea), togaviruses (alphaviruses, flaviviruses, and rubella virus causing epidemics of fever, yellow fever, dengue haemorrhagic fever, Japanese encephalitis and rubella), orthomyxo-virus (influenza A, B, C), paramyxovirus (measles and mumps), rhabdovirus (rabies), retrovirus (HIV), and arena-virus (Lassa fever in Lassa, Nigeria). HIV means Human Immunodeficiency Virus. HIV is the cause of AIDS (ie, Acquired Immune Deficiency Syndrome). HIV triggers a progressive and irreversible depletion of T-helper lymphocytes (Chapter 32). The lack of immune defence in HIV-patients make them easy victims to opportunistic infections and cancer, which often occur simultaneously. The transmission pathway is sexual contact - both homo- and hetero-sexual - or through parenteral exposure to blood. Opportunistic infections in AIDS are caused by bacteria & mycobacteria (Legionella, Listeria, Salmonella, Shigella, TB), viruses (Cytomegalovirus, Herpes Simplex, Varicella-Zoster), fungi (Candida, Histoplasma, Cytococcus), and protozoa (Entamoeba Histolytica, Pneumocyctis Carinii, Toxoplasma). The asymptomatic HIV patient is typically attacked by pneumonia (Pneumocystis Carinii), which must be treated carefully. Alternatively it is terminal. There is oral candidiasis, recurrent diarrhoea, and progressive demyelinisation of CNS (ie, leuco-encephalopathy). Viral hepatitis is an infection of the hepatocytes causing cell destruction (necrosis) and inflammatory reactions. The five hepatitis viruses are marked A, B, C, D, and E. Also yellow fever virus, Epstein-Barr virus (infectious mononucleosis), cytomegalovirus, rare enteroviruses, herpes simplex virus, rubella virus, and Ebola-virus can cause hepatitis. Hepatitis A virus (HAV) is a small picornavirus, which is only replicated in hepatocytes, excreted with the bile and found in the faeces of infected patients. HAV is evidenced in the faeces for 3 weeks just before the onset of the jaundice and a week after. The virus is directly cytotoxic but probably also acts by immuno-mediation such as helping natural killer cells to kill hepatocytes. Following a relatively short incubation period, the patient develops increasing fatigue, lack of appetite, vomiting, diarrhoea and fever. Abdominal pain may simulate acute abdomen, but soon the jaundice is diagnostic. When the icteric phase begins there is often subjective improvement. The urine becomes dark with green foam by bilirubin, and the stools are pale owing to intrahepatic cholestasis. The liver damage is shown by a rise in aspartate serum amino-transferase (AST) and 5 weeks from the exposure there is a rise in IgM anti-HAV in the blood. The latter is an indicator of acute infection, and soon disappears. As the patient recovers more and more IgG anti-HAV appears and persists for life. Complete recovery is followed by lifelong immunity. Hepatitis B virus (HBV) is a hepatotropic virus, which was the first member of the group, termed hepadnavirus. HBV probably affects the hepatocyte by immunological processes without being directly cytotoxic. HBV consists of a shell and a core. The shell expresses an antigen called Hepatitis B surface Antigen (HBsAg), which is secreted into the blood plasma from the infected hepatocyte. The core of the virus contains double-stranded DNA, DNA polymerase, and immunogenic material termed core Antigen (HBcAg) and a degradation product of HBcAg called e Antigen (HBeAg). Many cases are asymptomatic, other cases show a clinical course like the HAV infection, and still others show a fulminant pattern or end in chronic hepatitis. Complete recovery is typical, but all recovered patients are potential carriers. HBV is spread by blood or blood products and is also found in semen and saliva. The intravenous route includes blood transfusion, contaminated needles, or sexual contact. HBsAg appears in the blood even before the onset of symptoms. Typically, the recovery is rapid and HBsAg disappears again, but now antibodies to HBsAg (IgM anti-HBs) appear. These IgM anti-HBs molecules provide lifelong immunity, and are lifelong markers of previous HBV infection. Also IgM anti-HBc, the antibody to HBcAg, is a useful marker of previous HBV infection, probably without protective functions. HBeAg appears in the blood while the infection is severe, and declines rapidly in recovery. If HBeAg remains in the blood it usually expresses fulminant viral replication. IgM anti-HBe appears as the HBeAg disappears from the blood, and their presence indicates a relative improvement of hepatocyte function. Precipitation of immune complexes (HBsAg- IgM anti-HBs) sometimes causes serum sickness, with glomerulonephritis, polyarthritis, pancreatitis, and urticarial rashes. Chronic hepatitis is hepatic failure with sustained antigenaemia (ie, HBsAg) for more than 6 months. Chronic hepatitis B patients carry a significantly increased risk of liver cirrhosis and hepatocellular carcinoma. Hepatitis C virus (HCV) is a 60 nm large RNA flavovirus, which is responsible for most cases of post-transfusion hepatitis. The clinical course is discrete or asymptomatic, but later many patients develop chronic hepatitis. HCV antigens produce antibodies, which are found in the blood plasma (IgM anti-HC). Some cases are treated with interferon-a. Hepatitis D virus (HDV) is an RNA virus frequently affecting drug abusers. In the blood HDV is coated with HBsAg, and HDV infection is thus associated exclusively with HBV co-infection or with HBsAg-positive patients. The clinical course is like acute HBV infection, but sometimes fulminant or fatal. Diagnosis is confirmed by a blood sample showing IgM anti-D together with IgM anti-HBc. Hepatitis E virus (HEV) is an RNA calcivirus, which causes a water-borne hepatitis. Epidemics have occurred among risk groups for HBV infection and in developing countries. Good hygiene is essential, and boiling of water for at least 10 min is necessary in areas with contaminated water. The therapy of viral hepatitis is symptomatic. Prevention by avoidance of risk factors and immunisation is the only rationale. Chronic HBV carriers can be treated with interferon-a, which may reduce the risk of later development of hepatic cirrhosis and hepatocellular carcinoma. Yeast reproduces by budding, whereas moulds grow by branching hyphae. Histoplasmosis, cryptococosis, blastomycosis, and candidiasis are all systemic infections, which can be treated with the polyene, amphotericin, which kills young growing cells. Histoplasmosis and cryptococcosis are world-wide mycoses caused by Histoplasma capsulatum and Cryptococcus neoformans (yeast fungi). The reservoir for the spores is bird and bat droppings and wet soil. The clinical features of pulmonary mycosis are like pulmonary tuberculosis with a tendency for fistulae. Cryptococcosis usually presents as meningitis. Candidiasis is caused by Candida albicans - the most common fungus in humans mainly occurring as vaginal infections and oral thrust. Blastomycosis is primarily a skin disease caused by blastomyces dermatitidis. Pulmonary lesions look like TB or malignancy on X-rays. Dermatophytoses affect the skin, hair and nails (Trichophyton, Microsporum, and Epidermophyton). Different types of Leishmania cause leishmaniasis. The protozoa are transferred via the sandfly. It invades the reticuloendothelial cells, and replicate before they spread to cause bone marrow hyperplasy, hepatomegaly, lympadenopathy, and splenomegaly. Visceral Leishmaniasis is called Kala-azar. Malaria (meaning bad air) in 1897 was found to be caused by the parasite, plasmodium, found in the stomach of mosquitoes. Four species of Plasmodium exist: The malignant, virulent P. falciparum, and the three less virulent P.malariae, P. ovale and P. vivax. Malaria is said to have spoiled civilisations throughout history. The parasites are transmitted by female Anopheles-mosquitoes, by infected drug syringes or by blood transfusion. As the mosquito bites, the parasite enters a red cell and multiplicate. Phagocytosis of parasitized red cells leads to reticuloendothelial hyperplasia with hepato-splenomegaly. P. Falciparum can invade red cells at any age and is the most malignant type, because of red cell haemolysis. A new mosquito sucks blood-containing parasites from the patient. The parasites multiply in the stomach and salivary glands of the mosquito. The next mosquito bite of a new victim is the start of a new life cycle for the parasite. The incubation period is around 2 weeks. Cerebral malaria is characterised by attacks of extremely high body core temperature, convulsions, coma, and possibly death. The attacks occur each 2. or 3. day when the parasites synchronously leave the red cells and spread into the blood. Blackwater fever is named after the black urine caused by intravascular haemolysis. Encephalopathy, congestive heart failure, pulmonary oedema, emboli, and renal failure may develop into a terminal crisis. Elimination of mosquitoes has failed to prevent malaria. In several regions of Asia, the parasite is resistant to all traditional antimalarial drugs, because the parasites can change their coating, so the host immuno-defence system does not work. Toxoplasmosis is caused by infection with the intracellular Toxoplasma gondii. There are many mammals functioning as intermediate hosts but the final host is the cat. Infection occurs by ingestion of food contaminated by Toxoplasma gondii cysts. Sulphadiazine and the diaminopyrimidine, pyrimethamine, for one month is effective as a synergistic therapy. Trypanosomiasis is found in Africa (sleeping sickness) and in South and Central America (Chagas disease). The African Trypanosoma brucei is transmitted by both male and female tsetse flies, whereas various insects transmit the American Trypanosoma Cruzi. First there is a tender nodule at the site of the bite. Then the protozoa invade the lymphatic system and finally the blood. In sleeping sickness the protozoa reach all organs of the body but the CNS is particularly occupied. A meningo-encephalomyelitis develops, where the patient becomes apathetic and sleepy. In Chagas disease there is regional lympadenopathy, fever, hepatomegaly, and myocarditis. Chronic Chagas disease is an autoimmune disorder caused by T-cells and antibodies against vital organs (cardiac failure, emboli). The helminths are divided into three groups: 5a. Roundworms (ie nematodes), 5b. Flukes (ie trematodes, flatworms), and 5c. Tapeworms (ie cestodes, flatworms). 5a. Nematodes or roundworms are divided into intestinal (Ascaris lumbricoides, Enterobius vermicularis or pinworm, Trichinella spiralis, Tricuris trichiura or whipworm, and the hookworm or Anchylostoma duodenale/Necator americanus), and extraintestinal roundworms (filariae or Wuchereria bancrofti/Brugia malayi, Loa loa or eyeworm, Onchocerca volvulus, and Dracunculus mediensis or guinea worm). 5a.a. Ingestion of infective eggs is the usual cause of infection with intestinal roundworms. Identifying eggs in the faeces makes the diagnosis. Ascaris lumbricoides causes ascariasis, where adult roundworms attach to the small intestine, and pregnant worms discharge eggs that are expelled with the faeces. In moist soil the eggs become infective within a month. When ingested in food or water, the eggs hatch, and the larvae enter the portal blood. The larvae pass with the blood through the liver and heart, reach the lungs and develop into 3.th stage larvae. They ascend up the trachea, down through the alimentary tract and stay in the small intestine, where they mature. Massive infections cause intestinal obstruction, appendicitis and malnutrition. Eggs can also be deposited in other tissues. Enterobius vermicularis (pinworm) causes enterobiasis, where the worms live in the colon. Pregnant worms migrate through the anus and deposit eggs in the perianal region, where the victim experiences anal pruritus. Humans ingest the infective eggs, they hatch in the intestine and the larvae mature in the colon. Trichinella spiralis Trichinella spiralis is transmitted, when we are eating undercooked or raw meat (pig) containing encysted larvae. During digestion the encysted larvae are liberated and mature into adult worms that attach to the mucosa of the small intestine. The worms then discharge larvae that reach the blood stream and penetrate the vessel walls to be encysted in striated muscle. This may cause muscle pain, oedema, eosinophilia and fever. The larvae also migrate to the heart, the lungs and the nervous system. Tricuris trichiura (whipworm) The whipworm infects humans when ingesting their eggs in food and water. The eggs hatch larvae in the gut and they mature into adults in the colon, where they thread their whip end into the mucosa. Massive infection causes abdominal pain including acute abdomen with appendicitis or diarrhoea with bloody stools. The loss of blood leads to anaemia. Hookworm (Anchylostoma duodenale/Necator americanus) The hookworm larvae survive for months in soil protected from direct sunlight. The larvae penetrate the skin of humans and enter the blood. In the lungs they migrate to the alveoli, ascend to the epiglottis, and are swallowed. In the intestine they attach to the mucosa with their toothlike hooks and eat the villi. The bleeding leads to anaemia, and the skin and lung lesions result in dermatitis and pneumonitis. 5a.b. The extraintestinal roundworms penetrate the skin. The diagnosis is established by microfilariae in the blood or by filariae in biopsies. Filariae (Wuchereria bancrofti/Brugia malayi) These parasites cause filariasis. Both filariae live in and block lymph vessels near the testes. Lots of different mosquitoes are intermediate hosts and humans are the final host. Symptoms are due to blockade and dilatation of lymphatic vessels to the testis, the epididymis and the spermatic cord. The tissue is inflamed with accumulation of lymphocytes, eosinophils and plasma cells. Pregnant filariae discharge microfilariae to the blood, where they may cause thrombo-embolism and create pulmonary infiltrates. The lymphoedema of the extremities results in elephant legs and is called elephantiasis. Loa Loa (eyeworm) The Loa Loa worm causes the African loiasis. Mango flies transmit the infection, and human are the definitive host. The worm migrates through the skin or the conjunctiva of the eye. Pregnant worms discharge microfilariae into the blood. Dermal swellings of worms surrounded by inflammation are typical findings. Worms can be extracted beneath the conjunctiva. This worm causes onchocerciasis, which is transmitted by blackflies and man is the ultimate host. The adult worm is coiled up in the subcutaneous tissue and form inflammatory nodules. Pregnant worms discharge large amounts of microfilariae, which migrate, to the eyes, lymph nodes and other organs. In the eye the microfilariae cause inflammation and blindness, and in the inguinal lymph nodes they cause genital elephantiasis. Dracunculus mediensis (guinea worm) The guinea worm is transmitted with water contaminated with an intermediate host, a crustacean of the type Cyclops. The adult worm lives in the subcutaneous tissue and cause urticaria with blisters. The blisters burst in contact with water and a multitude of larvae are discharged from the pregnant worm into the water. Treatment of intestinal and extraintestinal roundworms is performed with antibiotics (mebendazole, thiabendazole), that inhibit glucose transport and protein secretion in the worms. 5b. Flukes (trematodes) are found in the blood, the intestine or in the lungs. The most important flukes are the blood-dwelling Schistosoma haematobium, S. japonicum and S. mansoni. The intermediate hosts are fresh-water snails. Schistosomiasis (Bilharziasis) presents with swimmers itch at the site of invasion of the parasite. The blood to the heart, lungs and liver transports the cerariae. Eggs surviving in the mesenteric venules, the liver, and the urinary bladder cause most of the clinical manifestations. Generalized allergy develops with urticaria, asthma, eosinophilia, myalgia and fever. The patient eventually develops pneumonia, hepatosplenomegaly and lympadenopathy. The life cycle of the parasite is complicated. The adult worms reside in pairs with the female lying in the gynecophoric canal of the male. The pair copulates and produces several hundred eggs daily in humans. Within the egg a larval form, miracidium, develops. The schistosome eggs must leave the body to complete the life cycle of the parasite, and they penetrate the intestinal wall or the bladder wall to be expelled with the faeces or the urine. On contact with fresh water the miracidiae hatch from the eggs and find a snail, which they penetrate. In the snail they multiply enormously, and thousands of infective cerariae are expelled daily. During swimming or contact with water, humans are infected by cerariae penetrating the skin or mucous membranes. Flukes are treated with praziquantel, which destroys the surface of the worm, after which the worm is killed by host killer cells (see above). 5c. Tapeworms (Cestoda) Many tapeworm infections are asymptomatic. Taenia saginata (beef tapeworm), T. solium (pork tapeworm), Diphyllobotrium latum (fish tapeworm), and Hymenolepsis nana (dwarf tapeworm) all live within the human intestinal tract. When human ingests the T. solium eggs from human faeces and become infected with cysticerci, a serious condition - called cysticercosis - is in progress. The eggs release larvae, which enter the blood, remain in different tissues, and develop into an intermediate larval form, the cysticercus that can survive indefinitely. The cysticercus grows and compresses the surrounding tissues. In the brain the cysticerci may cause hemiplegia or epilepsy, and in the eye they may cause blindness Tapeworms are also killed by praziquantel (see above). 6. Sexually related infections Gonorrhoea, Clamydia, Herpes simplex, Trichomoniasis, Candidiasis, hepatitis, HIV and AIDS, syphilis, yaws, Bejel and pinta are sexually related infections already described above This paragraph deals with Chancroid, Lymphogranuloma venereum, Granuloma inguinale, Scabies, and Pediculosis pubis. Chancroid or soft chancre (ulcus molle) is a venereal disease caused by a short bacillus, Haemophilus Ducreyi. The ulcer is soft and extremely tender in contrast to the hard syphilitic chancre. The bleeding ulcers may transfer HIV infection. The bacillus grows on special culture media, but it is fastidious. Cephalosporins and quinolones may prove effective. Lymphogranuloma venereum is caused by Chlamydia trachomatis (besides trachoma, see above). The ulcer is painless, and the inguinal lymph nodes grow. Oxytetracycline is necessary. Granuloma inguinale is caused by Calymmato-bacterium granulomatis, which is identified with the microscope. Erythromycin or tetracycline is effective. The mite, Sarcoptes scabiei, causes scabies. A skin lotion with Malathion is applied. Malathion is a widely used pesticide that works as an anti-choline-esterase and kills the eggs of mites and lice. Pediculosis pubis or pubic lice is a venereal disease, where lice are found in the pubic hair or in all hairy areas. The eggs are killed with Malathion, which is safer than other pesticides. Genital ulcer diseases associate with HIV infection, and their cure is important in the prophylaxis against spread of AIDS. Each of the following five statements have True/False options: A. Prostaglandins are important for the inflammatory reaction, and they are products of cyclo-oxygenase activity. ASA and corticosteroids inhibit the synthesis. B. The maximal reabsorption of NaCl and water occurs in the distal tubule of the nephron, and is driven by the Na+-K+-pump. C. Japanese encephalitis is caused by a flavivirus and is transferred by mosquitoes. D. Acyclovir inhibits viral DNA synthesis, and is effective enough to kill HIV. E. Influenza is not a clinical entity caused by influenza virus A, B and C, only. Infection with other viruses can produce the same clinical picture. A male comatous patient is brought to the city hospital in Patuakhali (at the river, Ganges). The patient is 1.80 m tall, but is obviously dehydrated. His normal body weight is 75 kg, and his weight at admittance is 60. The normal extended extracellular fluid volume is 20% of the body weight (Chapter 17). There is a severe rice-water diarrhoea of more than 1 litre in the first hour. Motile vibrios are demonstrated in the microscope by dark-field illumination, and the motility is reduced with vibrio cholerae antiserum. The haematocrit is 60%, serum Na+ is 120 mM and the Base Excess is -15 mM. The pHa is 7.17 and PaCO2 is 33 mmHg (4.4 kPa). The patient is immediately treated with intravenous infusion of the WHO diarrhoea treatment solution. This is 68 mmol NaCl (4 g), 13 mmol KCl (1 g), 50 mmol glucose( 9 g), and 80 mmol sodium acetate (6.5 g) dissolved in 1 litre of water. The rehydration has a dramatic effect following 2 litres of infusion. The patient is awake and complains of thirst. The Base Excess is now -8 mM, the pHa is 7.33 and PaCO2 is 31 mmHg (4.14 kPa). The patient is also given tetracycline for 3 days, which cure the condition, and he is released from hospital after 4 days. The last two days he only receives an oral glucose-electrolyte solution. 1. Describe the pathophysiology of cholera. 2. Describe and calculate the normal extended ECV at the start of the disease. 3. What is the fractional loss of extended ECV per hour? 4. Is rehydration important? 5. What is the effect of tetracycline? 6. Calculate the number of base equivalents missing in the normal extended ECV. The approximate amount was included in the first 2 litres of infusion. Why was this amount insufficient (change of base excess from -15 to -8 instead of zero)? A 22-year old male returns from Africa, where he has been travelling for 6 weeks. Two weeks later he is not at work, and he does not answer the telephone. A friend goes to his flat, where newspapers are piled in front of the door, and there is no reply. The police and a key expert are called, and when entering the rooms they find the young man in coma. Immediate admission to the emergency department is arranged. Here the core temperature is recorded to 40.8oC. The hospital doctor institutes a series of tests and calls the patients GP in order to get relevant information. He is informed that the patient before going to Africa was vaccinated against hepatitis A, typhoid, tetanus, and meningococcal meningitis. The patient was also instructed about malaria prophylaxis and advised to take 300 mg chloroquine each Sunday during the travel and continue for 7 weeks after returning home. 1. What is the probable diagnosis? 2. How are the diagnosis confirmed? 3. What are the proper treatment? A male refugee from ex-Yugoslavia , 36 years old (weight 69 kg, height 1.82 m), is examined by a doctor at the refugee camp, because of coughing and shortness of breath. He has lost 7 kg in weight recently. There has been night sweats and sparse mucous blood-stained sputum. During auscultation a few crackles are heard over both lungs. The patient has never smoked. The patient lives in close quarters with many people, and he is admitted to hospital for further examination. The peak expiratory flow is measured to 510 l min-1. A chest X-ray shows patchy shadows in the upper zones of both lung fields. Two of the shadows are calcified. Sputum is stained with the Ziel-Nielsen stain, but no acid and alcohol-fast bacilli are found. Gastric juice is aspirated at 3 occasions. The gastric juice is cultured on Løwenstein-Jensen medium for 4 weeks, where characteristic acid and alcohol-fast bacilli are found after Ziel-Nielsen staining. 1. What is the diagnosis? 2. What are the treatment? 3. Does this patient benefit from steroid therapy? 4. What are the necessary screening procedures for the persons living with the patient before he was sent to hospital? Try to solve the problems before looking up the answers . · Antibiotics have toxic effects, especially when used in overdose or in the presence of other disease such as hepatic or renal failure. Aminoglycosides are both oto- and nephro-toxic. · Antibiotics can lead to secondary infections with fungi or with Clostridium difficile. · Serious bacterial infections (eg, endocarditis, meningitis, TB, septicaemia) and infections in immunodeficient patients are commonly treated with bactericidal drugs (aminoglycosides, cephalosporins, and penicillins). Such serious infections are preferably treated with combinations of synergistic antibiotics. · The advantages of cephalosporins over penicillins are their resistance to penicillinase and their wider antimicrobial spectrum (both Gram-positive and Gram-negative bacteria). · Aminoglycosides, chloramphenicol, clindamycin, erythromycin, fusidic acid, mupirocin, spectinomycin, tetracycline all bind to bacterial ribosomes and interfere with protein synthesis. · Fusidic acid has a bile acid structure and inhibits Gram-positive cocci including penicillinase-producing Staphylococcus aureus in combination with other antibiotics. · Idoxuridine and vidarabine is used as early as possible against herpes simplex virus and against varicella zoster virus (herpes zoster and severe varicella or chickenpox). · Acyclovir inhibits viral DNA synthesis and is effective against the same virus disorders. · Azidodeoxythymidine inhibits HIV reverse transcriptase and thus impairs viral replication. This substance is used for HIV patients, although there is danger of bone marrow depression. · Interferon is produced by the T-lymphocytes during virus infections. Interferon is used for hepatitis B and C. · Leishmaniasis is treated with meglumine antimoniate and Na-stibogluconate. These substances inhibit phosphofructokinase and Krebs cycle enzymes in the Leishmania organism. · Malaria is caused by infection with the Plasmodium protozoa, which is present in the human host in the blood (erythrocytic) or the tissue (extraerythrocytic stage. The erythrocytic stage is treated with aminoquinolines (eg chloroquine) or analogues. · Chagas disease is treated with nifurtimox, which produces free radicals. The free radicals react with oxygen to form superoxide anion, hydroxyl-free radical, and hydrogen peroxide. The trypanosomes do not contain enzymes able to inactivate these reactive substances, so they cause peroxidation of lipids and ribonucleic acids (DNA, RNA). · Roundworm disorders are treated with mebendazole or with thiabendazole. These substances bind to the cytoplasmic microtubules of the roundworm and inhibit glucose transport and protein secretion. · Flukes are sensitive to praziquantel, which attacks the surface barrier (tegumentum) and the muscles of the worm. Praziquantel destroys the surface of the worm so host antibodies can bind to the worm antigens. · Tapeworms are also killed by praziquantel, but as an alternative the tapeworms are sensitive to niclosamide. Niclosamide binds to the mitochondria of both host and parasite and block ATP formation. · Cholera is a disease caused by an enterotoxin produced by the gram-negative bacillus, vibrio cholerae. If this bacillus is allowed to proliferate within the lumen of the small intestine, it causes profuse watery diarrhoea - up to 24 l per 24 hours - dehydration and circulatory shock. Fulminant cholera can kill the patient within a day. · Plague is spread from woodland rodents to domestic rats. The rat flee bites humans. Bubonic plague occurs suddenly with high fever and the patient is confuse and may seem drunk due to toxaemia. The inguinal lymph nodes rapidly develop lympadenopathy or buboes. Pneumonic plague is fulminant pneumonia with bloody sputum and cardiac failure. · Syphilis (Lues) is caused by Treponema pallidum, which is a mobile spirochaete. Congenital syphilis is acquired transplacentally from mother to foetus and is apparent a few weeks after birth. The babies pass through three stages of the disease similar to those of the adults. Adult syphilis is acquired by intimate sexual contact. · Flukes (trematodes) are found in the blood, the intestine or in the lungs. The most important flukes are the blood-dwelling Schistosoma haematobium, S. japonicum and S. mansoni. The intermediate hosts are fresh-water snails. Schistosomiasis (Bilharziasis) presents with swimmers itch at the site of invasion of the parasite. · Taenia saginata (beef tapeworm), T. solium (pork tapeworm), Diphyllobotrium latum (fish tapeworm), and Hymenolepsis nana (dwarf tapeworm) all live within the human intestinal tract. When humans ingest the T. solium eggs from human faeces and become infected with cysticerci, a serious condition - called cysticercosis - is in progress. Clinical infectious Diseases. Monthly journal published by the Infectious Diseases Soc., University of Chicago Press, Journals Division, PO Box 37005, 5720 South Woodlawn, Chicago IL 60637, USA. Dhein S, Vann Koppen C J, and O-E Brodde. Muscarinic receptors in the mammalian heart. Pharm Rev 44, No3, 2001. Mims C, Playfair J, Wakelin D, and R Williams. Medical Microbiology. 4th Ed. Mosby, London, 2007.
|
||
Click here to introduce your comments or contributions