New Human Physiology | Paulev-Zubieta 2nd Edition
Chapter 12: Blood FLow, Distribution and Shock
| HOME | PREFACE | TABLE OF CONTENTS | SYMBOLS | SECTION INFO | CONTRIBUTORS | LINKS | CONTACT US |
Highlights
Study_ObjectivesPrinciplesDefinitionsEssentials
PathophysiologyEquationsSelf-AssessmentAnswers
Further Reading
|
Chapter 12
|
 |
|
|
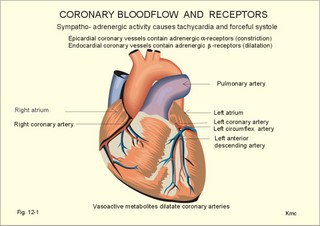
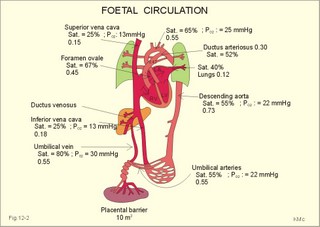
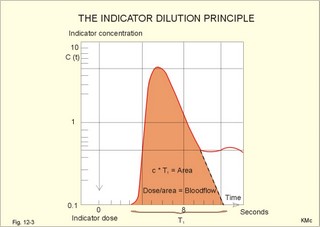
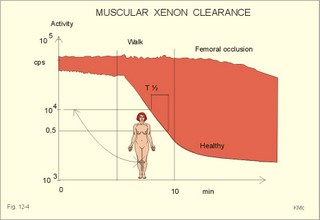
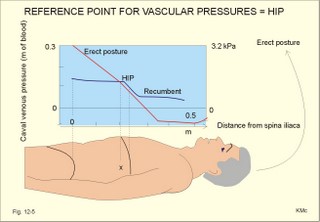
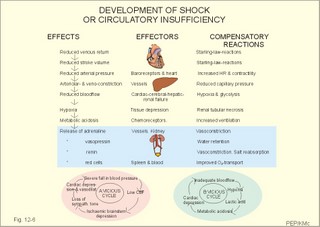
· To define concepts such as anaphylactic shock, bloodflow, hydrostatic indifference point, hypotension, mean circulatory equilibrium pressure, mean transit time, and shock. · To describe the principle of mass balance (Fick principle) for cardiac output determination, the dilution principle (tracer or indicator bolus), the isotope-wash-out-method, the venous occlusion plethysmography, and the mean transit time method. · To draw an indicator dilution curve, an isotope-wash-out-curve and a plethysmography curve with flow determinations. · To calculate one variable when relevant information is given. · To explain the control of bloodflow to the brain the myocardium, the kidneys, the muscles, the gastrointestinal channel, the skin, and the foetus. To explain the compensatory reactions to shock. To explain the cerebral ischaemic response. · To use the concepts in problem solving and case histories. · The law of conservation of matter (see Chapter 8). This principle is used to measure bloodflow. · Fick´s principle for determination of cardiac output (see Chapter 10). · Poiseuille´s law. When the radius of a vascular bed is doubled, its bloodflow may increase by as much as 16 times. This is because of Poiseuille´s law (see Eq. 8-3). · Anaphylactic shock (anaphylaxis) refers to a severe allergic disorder in which the cardiac output and the mean arterial pressure fall rapidly and drastically (see Chapter 32). · Hydrostatic indifference point is the point in the cardiovascular system, in which the pressure does not change with change of body position. · Hypotension. Severe hypotension refers to a condition with a systolic blood pressure below 75 mmHg (10 kPa). · Mean circulatory equilibrium pressure is a pressure of 1 kPa measurable in all divisions of the circulatory system just after cardiac arrest. · Mean transit time for indicator particles in a system is equal to the sum of all transit times for all single particles divided with their number. · Shock is a clinical condition characterized by a gradual fall in arterial blood pressure and rapid heart rate. Respiration is also rapid and the skin is moist, pale or bluish-grey. · Vasovagal syncope or emotional fainting is a condition, where the fainting is caused by a strong emotional activation of the parasympathetic nervous system via the hypothalamus with bradycardia, vasodilatation and decreasing arterial pressure. This paragraph deals with 1. The coronary bloodflow, 2. The regulation of coronary bloodflow, 3. Brain bloodflow, 4. Skin & fat bloodflow, 5. The splancnic circulation, 6. The foetal circulation, 7. Fick’s principle, 8. The dilution principle, 9. Clearance, 10. The isotope-wash-out-method, 11. The mean transit time, 12. Vascular pressure reference (supine to standing). The myocardial metabolism is an exclusively aerobic process under normal conditions. It depends on oxidative phosphorylation in order to re-synthesise ATP. The O2 needs of the myocardium are therefore great, even at rest. Exercise can increase the needs six-fold; however, the myocardium cannot extract a greater fraction of the O2 delivered, since the myocardial O2 extraction is already close to maximum at rest. Thus the coronary bloodflow must rise importantly during exercise in order to deliver the O2 needed. Two main coronary arteries arise from the aorta. The left main coronary artery (Fig. 12-1) divides into two major branches: The left anterior descending artery, which courses down the interventricular groove towards the apex of the heart, and the left circumflex artery, which courses leftward and posteriorly in the atrioventricular groove to the postero-lateral wall of the left ventricle. The right coronary artery (Fig. 12-1) arises from the right aortic sinus and courses rightward and posteriorly in the atrioventricular groove to reach the right atrium, and via the posterior descending artery to the posterior wall of the left ventricle and the lower part of the interventricular septum. Later the right coronary artery also gives off branches to the posterolateral wall of the left ventricle. This arrangement of coronary vessels exists in half of the population in western countries. In 30% of the population the posterior descending artery arises from the right coronary artery, and the posterior left ventricular branch arises from the left circumflex artery. In another 20% of the population the right coronary artery is small and supplies only the right atrium and the right ventricle with blood, and all the blood supply to the left ventricle comes from the left main coronary artery. The main arteries run along the epicardial surface and divide several times on the surface of the heart before they send off small penetrating vessels forming a network of intramural arteries, arterioles and capillaries in their way to the endocardium. The myocardial capillaries feed into a net of intramural venules. They drain eventually into the epicardial collecting veins. Right ventricular venous blood drains into the right atrium. Left ventricular venous blood drains into the coronary sinus that empties in the right atrium, except for a small blood volume, which drains into the left ventricle. The epicardial coronary vessels contain a preponderance of constrictor receptors called adrenergic a-receptors, whereas the intramuscular and endocardial coronary receptors have a preponderance of dilatator receptors called adrenergic b-receptors. Fig. 12-1: Coronary bloodflow and receptors. Due to the contraction of the myocardium in systole, the myocardial bloodflow is blocked and the heart receives its nutrition in the diastolic period (Fig. 10-7). The coronary bloodflow is phasic. 2. The regulation of coronary bloodflow The coronary bloodflow is described before in Chapter 9 (paragraph 3) and in relation to Fig. 10-7. The coronary bloodflow is mainly controlled by local metabolic autoregulation, and sympathetic stimulation does not always cause significant vasoconstriction. Accordingly, a moderate decrease in arterial blood pressure down to 9.3 kPa (70 mmHg) does not significantly reduce the bloodflow through the myocardium. Unlike skeletal muscle tissue, the myocardium cannot function anaerobically for extended periods by building up an oxygen debt. Thus, oxidative ATP synthesis must continuously match ATP utilisation in the heart. At rest the heart produces 70% of its ATP from oxidation of fatty acids and 30% from oxidation of carbohydrates. During exercise with lactate production by skeletal muscles, this lactate becomes an important substrate for the myocardial metabolism, entering the tricarboxylic acid cycle after conversion to pyruvate. Catheterisation of the venous sinus of the heart in healthy subjects at rest reveals a venous haemoglobin saturation fraction of 0.30. Hence, 0.7 parts of the haemoglobin concentration of the venous blood is desaturated. Thus, arterial blood with a normal oxygen concentration (Cao2 of 200 ml per l) liberates (200 × 0.7) or 140 ml of oxygen per l to the myocardium. Variations in the arteriovenous O2 content difference at the steep part of the O2-haemoglobin dissociation curve can only change the myocardial O2 tension modestly. The extremely high O2 content difference of the heart at rest implies that a rise in coronary bloodflow must be the main source of extra O2 to the heart during exercise. Most of the blood entering the coronary circulation is delivered during the diastolic phase. This is because the myocardial tissue pressure increases during systole, and the contraction squeezes the blood/myocardium - in particular in the subendocardial layer. Therefore, the systolic bloodflow through the inner layer of the left ventricular wall approach zero. The duration of each diasole is reduced with increasing heart rate, so the increased oxygen demands during exercise calls for a higher coronary artery pressure in diastole in order to secure the necessary bloodflow. The blood reaches the brain through the internal carotid and the vertebral arteries. The dominant control of cerebral bloodflow (CBF) is metabolic autoregulation but also a pressure dependent myogenic autoregulation is present. The smooth muscle walls of the small cerebral arteries respond immediately to changes in the transmural pressure gradient. Hereby, the CBF is maintained constant despite changes in systolic blood pressure between 80 and 160 mmHg (10.7-21.4 kPa). The small brain vessels are metabolically regulated. Increased PaCO2 and reduced PaO2 dilatates brain vessels and increase CBF. CO2 (not H+) passes the blood-brain barrier easily. The mean arterial pressure can double without any appreciable rise in CBF. A neuropeptide released in response to transient hypotension (calcitonin gene-related peptide) is probably involved in the autoregulation. The vertebral arteries join to form the basilar artery, which forms the circle of Willis together with blood from the internal carotids. When brain arterioles dilatate the CBF increases, and since the brain tissue within the cranium is relatively incompressible, the venous outflow must balance. CBF is normally 55 FU in humans at rest. One FU is one ml of blood per min per 100 g of brain tissue. With a normal brain weight of 1300 g this value corresponds to a total of (55 × 13) = 715 ml of blood per min. This resting CBF and the oxygen uptake of the brain can double during cerebral activity and triple in active brain regions during an epileptic attack (Chapter 7). The sympathetic nervous system plays a secondary role for the CBF. Some brain vessels contract by sympathetic stimulation. This neurogenic control only concerns the larger cerebral arterioles. Some degree of autoregulation is found in many other organs including the skeletal muscle mass, the splancnic area, and the kidneys. Blood flows through the skin and subcutaneous tissues in order to nourish the cells, and to regulate shell temperature. Blood flows much faster through the arteriovenous anastomoses in the skin of the face, the fingers and toes in a cold environment. The sympathetic activity constricts the metarterioles that lead to the skin, so the blood bypasses the cutaneous circulation. Hereby, the skin bloodflow can fall from about 5 FU´s and approach zero. The heat content of the blood returns to the body core, which helps to maintain the core temperature. In a warm environment, the sympathetic tone is minimal and the arterioles dilatate, so that the skin perfusion can rise to perhaps 70 FU, and much energy is given off to the atmosphere. Psychological influence can cause one to blush or to have a white face, by changing a-adrenergic constrictor tone and through the effect of local, vasoactive substances normally found in the skin. When a large fat combustion occurs (during hunger and distance running), the fat bloodflow can increase from 3 to 20 FU´s. Cold and warm environments alter the fat perfusion just like the skin perfusion (Chapter 21). The sympathetic regulation of the arteriolar tone in fat and skin tissue is also similar. The sympathetic change in tone is not related to the classical baroreceptors. The splancnic area is drained (1.5 l per min) via the hepatic veins at rest, so all blood passes through the liver. The liver receives more than one litre of blood from the portal vein and less than 0.5 l from the hepatic artery each minute. A special characteristic for the splancnic circulation is that two large capillary beds are partially in series with one another forming a portal system. The splancnic perfusion increases after meals, and decreases during fasting and duration exercise. The sympathetic nervous system has a tonic activity on splancnic vessels via a-adrenergic nerve fibres. Vagal fibres dilatate the splancnic vessels. Haemorrhagic shock can elicit a fatal splancnic hypoxia. The foetus depends completely on the mother and her placenta. The placental barrier can be passed by low molecular substances (nutrients, gasses and waste) by diffusion. The foetal haemoglobin (F) has a sigmoid dissociation curve, which is shifted to the left relative to haemoglobin A for adult, because haemoglobin-F has a greater affinity for oxygen than does adult haemoglobin (Chapter 15). Haemoglobin F is not affected by 2,3-DPG. Foetal blood has a high haemoglobin concentration (200 g l-1), so the foetus takes up large amounts of O2 in placenta. This occurs even at low PO2, and the maximal value in the placental blood is only 6.7 kPa or 50 mmHg. Often the foetus achieves an arterial oxygen concentration similar to that of the mother. Steroid hormones, maternal thyroid hormones, and catecholamines cross the placental barrier to the foetus. Peptide hormones cannot traverse the placental barrier, except small peptides such as thyrotropin-releasing hormones (TRH) and antidiuretic hormone (ADH). Foetal insulin contributes to anabolism and lipid storage. Human chorionic somatomammotropin, prolactin, and IGF-2 are the most important growth factors during foetal life. Foetal parathyroid hormone stimulates the transport of Ca2+ to the foetus. The maternal blood rich in O2 and nutrients is injected into the intervillous spaces of the placenta via spiral arteries, and returns with CO2 and waste to the mother via veins draining to the uterine veins. The chorionic villi dip into the internal sinuses of the placenta. The exchange of nutrients, metabolic waste and gasses across the placental barrier occurs by diffusion. Foetal blood rich in O2 and nutrients returns to the foetus from the placenta in the umbilical veins. The placenta has a diameter of 16-20 cm and the placental barrier has an area of about 10 m2. The blood flowing in the umbilical veins continues in the ductus venosus or the blood enters the foetal liver and then all blood is gathered in the inferior caval vein. The 80%-saturated blood from the umbilical veins flows into the foetus. The saturation is reduced to 2/3 (67%) when passing through the oval communication between the right and left atria (foramen ovale) to reach the left ventricle (Fig. 12-2). The blood in the left ventricle is mixed with desaturated blood from the lungs, whereby the oxygen saturation is reduced to about 65% in the blood passing to the upper-body foetal organs (brain and heart). The blood in the right ventricle (a mixture of blood mostly from the superior caval vein, but also the coronary sinus and the inferior caval vein to some extent) is only half-saturated. The foetal pulmonary vascular resistance is high due to the compressed inactive lungs (Fig. 12-2). Thus, the major part of the right ventricular output to the pulmonary artery bypasses the pulmonary circulation and flows through a foetal channel (ductus arteriosus) between the pulmonary trunk and into the descending aorta (Fig. 12-2). When the major part of the blood passes the ductus arteriosus and joins the left ventricular output, the resulting oxygen saturation is around 60% in the blood of the descending aorta reaching the lower part of the body and back to the placenta in the umbilical arteries. This shunt delivers well-saturated nutritive blood to upper-body foetal organs (brain and heart). Venous drainage from these essential organs returns to the foetal heart in the superior vena Cava. The right ventricle ejects the venous return. Much of the blood flowing in the descending aorta of the foetus is directed toward the placenta, so venous drainage from all organs is shunted toward the placenta, where wastes are eliminated from foetal blood, whereas O2 and nutrients are acquired. Maternal hypoxia and reduced venous return or pressure on the umbilical vessels during birth reduces the oxygen supply to the foetus, which is reflected as bradycardia. At birth, PCO2 increases, and the first breath reduces the intrathoracic pressure in the new-born, so placental blood is sucked into the baby (placental transfusion). When the bloodflow through the umbilical vein ceases, the muscular sphincter of the ductus venosus contracts. Massive sensory stimuli of the baby caused by labour and delivery, cutaneous cooling after delivery, the falling PAO2 and rising PACO2 without the placenta, and withdrawal of a placenta-produced respiratory inhibitor all adds up in activation of the respiratory centre and maintaining breathing in the newborn. The newly established air-liquid interface reduces pulmonary surface tension, which eases the lung expansion. Distension of the lungs with air also distends pulmonary vessels, so pulmonary vascular resistance (PVR) decreases drastically. Hereby, pulmonary bloodflow increases. As a consequence, bloodflow via ductus arteriosus slows, and pulmonary venous return to the heart increases (Fig. 12-2). Fig. 12-2: The foetal circulation. The left atrial pressure increases above that in the right atrium and the inferior vena cava by the newly established decrease in pulmonary vascular resistance, because of the large pulmonary bloodflow to the left atrium. Occlusion of the umbilical vein reduces the bloodflow to the right atrium, and occlusion of the umbilical arteries increases the resistance to the left ventricular output of blood. The resulting elimination of the pressure gradient across the atria, abruptly closes the valve over the foramen ovale, and the septal leaflets fuse within a couple of days. The low pulmonary vascular resistance reduces the pressure in the pulmonary artery, whereas the aortic pressure rises. This reverses the flow of oxygenated blood through the ductus arteriosus. Within minutes after lung expansion, the muscular wall of the ductus arteriosus constricts, and its closure is complete within 10 days. Failure of the foramen ovale or the ductus arteriosus to close gives rise to two congenital cardiac abnormalities (see later in this Chapter). Normal arterial blood gas tensions are established by 30 minutes of age. Left atrial pressure increases and foramen ovale closes soon after birth. This reverses the blood pressure gradient across the foramen ovale, so now the left atrial pressure exceeds the right. When the umbilical cord is closed, and the placental circulation is thus eliminated, the TPVR of the newborn increases. The decrease in pulmonary vascular resistance (PVR) and increase in TPVR means a great difference in the size of the blood pressures in the aorta and in the pulmonary artery. In conclusion, the parallel foetal circulation is transformed into a series circulation in the baby. The foramen ovale and ductus venosus close within 3 days of birth (Fig. 12-2). The sharp increase of O2 content (CaO2) in the baby's blood is a potent and universal vasodilatator. The dramatic changes in gas exchange affect cardiopulmonary and vascular regulation, probably via local mediators such as arachidonic acid and prostacyclin. According to the law of conservation of matter, mass or energy can neither be created nor destroyed (the principle of mass balance). Adolph Fick applied natural occurring indicators like O2 and CO2 when measuring cardiac output. Using O2 as an indicator and the law of mass balance, he claims that the O2 flux, taken up by the lung blood, plus the venous O2 flux to the lung, must be equal to the O2 flux, which leaves the lung in the oxygenated blood. Thereby, Fick proposed that the cardiac output could be calculated according to Eq. 12-1. A classical example of the usefulness of Fick's principle is to consider the data of a young healthy male at rest. The typical data for such a person are an O2 uptake of 250 ml STPD per min and an arteriovenous O2 content difference of 50 ml STPD per l of blood. According to Fick's principle, this male can only satisfy his O2 demands, if 5 l of blood is oxygenated in his lungs every minute. Thus, a cardiac bloodflow of 5 l per min is his cardiac output. The oxygen concentration of mixed venous blood is usually obtained through a venous catheter inserted up the median cubital vein, through the subclavian vein, and finally into the right ventricle or pulmonary artery, where the blood is well mixed. Arterial blood is easily obtained from the radial artery (CaO2). The disappearance rate of oxygen from the respired air can be recorded in a metabolic ratemeter as the oxygen uptake. The principle of mass balance is valid only for a system in steady state. Steady state is a state where the indicator is administered at a constant rate, and is neither stored, mobilised, synthesised nor used by the system, and where no shunts are present. This method has been used to measure a large increase in cardiac output in different patient groups. For example, patients with anaemia have been found to have higher cardiac output at rest. When an indicator bolus (mass or dose of tracer in weight or molar units) is instantaneously injected in the right side of the heart, the indicator and blood will mix. The mixture leaves the right ventricle through a well-mixed outlet, passes the pulmonary circulation and then returns to the left side of the heart. The indicator concentration during the first passage of any peripheral artery is recorded continuously or by multiple sampling. The resulting curve is shown in a semilog scale (Fig. 12-3). The indicator concentration (in mol/ml of blood) reaches a peak and then decreases in a few seconds, before it again rises due to indicator recirculation with the blood (Fig. 12-3). The first decrease in concentration is assumed to be mono-exponential. Hence it is easy to extrapolate to the concentration zero, and read the so-called first passage time, T1. In this case the T1 is 9 s (Fig. 12-3). The mean concentration ( c mol/ml) of indicator in the period T1 seconds is determined by planimetry. The average amount of indicator (in moles) leaving the left ventricle per second in one ml of blood is c, hence c is given in mol/ml of blood. The volume of blood (V) in which the indicator dose is distributed is dose/c. Since blood carries only c mol of tracer in each ml, the heart needs at least a bloodflow of V ml (dose in mol/ c) in order to carry the entire dose through the aortic orifice in T1 (9) seconds. Accordingly, the cardiac output per second is dose/(c*T1). The product (c*T1) is the area under the curve (Fig. 24-1). Thus the dose/area ratio must be equal to the bloodflow (ml/second) leaving the left ventricle. Put simply, the bloodflow (cardiac output in ml of blood per s or more convenient per min) can be measured by dividing the dose of indicator injected upstream by the area under the downstream concentration curve. Fig. 12-3: The indicator dilution principle. The bloodflow equation is also called the dose/area equation. An attractive choice of indicator is to use cold saline, of known temperature and volume. A flexible catheter, with a thermistor located at its tip, and an opening through which cold saline can pass, is used. The catheter tip is advanced to the pulmonary artery, while the opening supplies the right atrium with saline. The thermistor records the downstream alterations in temperature as the saline bolus passes. This is the thermodilution technique. This technique can be frequently repeated without having harmful effects. Moreover, there is negligible recirculation, and the method spares the patient the ordeal of an arterial puncture. This method is widely used. For example, interesting indicator dilution studies have shown the pump effect of external cardiac massage to be modest. Clearance is a theoretical tool for estimating bloodflow in the kidney and other organs. Clearance is the volume of blood plasma, which is totally cleared each minute of a given indicator by a specific organ (eg, renal clearance). The extraction (E) is the fraction of substance, which is extracted from the total amount transported to the organ per minute (Eq. 12-3). Clearance for para-amino hippuric acid (PAH) at low plasma concentrations is a measure of the renal plasma flow (RPF – see Chapter 25). The high hepatic extraction of bromsulphalein or of indocyanine is used to estimate the splancnic perfusion. 10. The isotope-wash-out-method A lipid-soluble indicator, such as 133Xenon dissolved in saline, is injected in the tibialis anterior muscle (* in Fig. 12-4 and Eq. 12-4). At steady state, the tracer concentration in the venous blood (Cv) is assumed to be the average blood concentration, and Ctis the mean tissue concentration. Fig. 12-4: Isotope (133Xe) wash out from the gastrocnemius muscle before, during and after walk on a treadmill. Upper curve is when the femoral artery is occluded - lower curve is from the healthy leg. The fractional fall in the mean tissue concentration of Xenon (Ctis) per time unit (dt) is constant during the whole elimination period (a rate constant = ln 2/T½). The flow/Wtis (weight of tissue) is a perfusion coefficient in FU (ml of blood per min and per 100 g tissue). The fall in mean tissue concentration per time unit (ratio dCtis/Ctis ) is measurable as T½ on the skin surface at the Xenon deposit in muscle tissue with a scintillation detector (Fig. 12-4 and Eq. 12-4). The method (see Eq. 12-4) is used clinically to detect peripheral vascular diseases. An example is intermittent claudication that refers to constricting pain arising during activity of any muscle group but most commonly in the calf muscles. The hypoxic pain and cramp appear after having walked a certain distance and is promptly relieved by rest. The cause is femoral occlusion due to arteriosclerosis with insufficient local bloodflow and ischaemic hypoxia (Fig. 12-4). The mean transit time (tmean) for indicator particles in a system with the volume, V, is equal to the sum of all transit times for all single particles divided with their number. This concept is used in a wide variety of indicator methods (Eq. 12-5). By means of intravascular catheters it is possible to measure the partial circulation time through most parts of the circulation. For a healthy adult at rest the normal ranges include the following: arm-ear 8-12 s, arm-lung 5-7s, and lung-ear 3-5 s. 12. Vascular pressure reference The heart is not always the correct reference point for blood pressure measurements. The elastic properties of the vascular tree differ throughout the body. Actually, the point in which the pressure does not change with change of body position is approximately 5 cm beneath the diaphragm during expiratory relaxation (Fig. 12-5). This is called the hydrostatic indifference point (HIP). Above this horizontal level, all vascular pressures are lower in the erect than in the recumbent position. The subatmospheric intrathoracic pressure counteracts venous collapse, so the intrathoracic veins remain open and the atrial pressures are zero in the erect position. The veins of the neck and face are collapsed. The venous sinuses of the brain are kept open by attachment to the surrounding tissues, and their pressures are around -1.3 kPa (-10 mmHg) in the erect position. Fig. 12-5: The hydrostatic indifference point (HIP) in an adult male. The subject changes position from recumbent to erect. HIP must not be mixed up with the mean circulatory equilibration pressure, which is a pressure of 1 kPa (6 mmHg) measurable in all divisions of the circulatory system just after cardiac arrest. This is also called the mean circulatory filling pressure, because it is a determinant of the venous return. When a supine person arise, his TPVR increases, the systolic blood pressure falls andthe diastolic blood pressure rises. Thus, the pressure amplitude falls, but the mean arterial pressure is unchanged. The stroke volume is reduced more than the heart rate rises, so the cardiac output will decrease when attending the standing position. An elegant way of studying circulatory consequences of standing is by use of lower-body-negative-pressure (LBNP). LBNP applied to a recumbent subject simulates the circulatory effects of standing. The venous return to the heart is dependent upon the body position, and upon the total blood volume. The venous return is also dependent upon the venous compliance and upon the sympathetic tone in the venous system and in the arteriolar system. When a person is located on a tilt table in a horizontal position, his blood pressures in a superficial vein on the feet is approximately 1.6 kPa (12 mmHg) and in the femoral veins 0.8 kPa (6 mmHg). When the person is turned upright towards the vertical plane, the venous pressure increases by the hydrostatic column up to the hydrostatic indifference point (HIP) just below the heart as long as he is not standing and using his skeletal muscle pump. If the tilt table is turned, so the head of the person is downward (Trendelenburg position), then the venous pressure increases in neck and head. The Trendelenburg position is rational during neck and head surgery. With the head upward the patient risks air embolism, if blood vessels are cut during neck and head surgery due to the subatmospheric pressure in the vessels. This paragraph deals with 1. Shock and 2. Congenital heart disease. Shock is defined as a clinical condition characterised by a gradual fall in arterial pressure and a rapid heart rate. Respiration is also rapid and the skin is pale, moist and grey. The general circulatory insufficiency causes the bloodflow to vital tissues to be inadequate, so delivery of oxygen and other nutrients as well as elimination of waste products is insufficient. In principle the circulatory insufficiency can be caused by disorders in the heart (cardiac insufficiency with imminent or manifest cardiogenic shock) or in the vessels (vascular insufficiency developing into vascular shock). The cardiogenic shock can be caused by restricted ventricular filling (bi- or tricuspidal stenosis, pericardial fibrosis, or cardiac tamponade); the cause can also be myocardial disorders (infarctions, myocarditis etc) or restricted/ineffective ventricular ejection in in cases wwith semilunar stenosis/insufficiency or shunts. The vascularly generated shock is caused by loss of blood or other fluids (absolute hypovolaemia) or by vasodilatation (relative hypovolaemia). Absolute hypovolaemia is caused by blood loss, plasma loss (burns or other denuding conditions, ascites, hydrothorax etc) or dehydration (water deprivation, severe diarhoea or vomiting, excessive sweating, intestinal obstruction with luminal fluid accumulation, urinary loss of proteins/salt/water, excessive use of diuretics, hypoaldosteronism etc). Relative hypovolaemia, sometimes with universal vasodilatation, is released by endotoxins (septic shock from viral or bacterial infections), anaphylactic shock (see Chapter 32) or by a neurogenic vasodilatation (neurogenic shock by severe pains or stress, anaesthetics or brain stem lesions close to the vasoconstrictor centre). The reduced delivery of oxygen and nutrients to virtually all cells of the body, is consequential: The mitochondria synthesise less ATP, the Na+-K+-pump operates insufficiently, the metabolic processing of nutrients is depressed which profoundly depresses muscular contractions, and finally digestive enzymes destruct the damaged cells. Glucose transport across the cell membranes in the liver and in the skeletal muscles is depressed including a severe inhibition of the actions of insulin and other hormones (Chapters 26 and 30). During progressive shock the metabolism is reduced and thus the heat energy, so the body temperature tends to decrease, if the patient is not kept warm. Compensatory mechanisms in shock are called negative feedback mechanisms, because they operate to counteract the fall in blood pressure. Baroreceptor responses and many hormonal control systems, that tend to raise the falling blood pressure, are examples of negative feedback (Fig. 12-6). The gain of a feedback system is defined as the ratio of the response to the stimulus itself. Decompensatory mechanisms exaggerate the primary fall in blood pressure. This is called positive feedback. A positive feedback mechanism can lead to a vicious cycle and death, if its gain is above one. Two examples with ischaemic brainstem depression and cardiac depression are shown in Fig. 12-6. Shock is divided into 3 stages by severity: 1A. Mild shock is a condition, where compensatory reactions can cure the patient without external help. A latent shock is produced when a healthy blood donor delivers more than the usual 500 ml of blood for transfusion, but the volume is often replaced within an hour. A number of negative feedback mechanisms oppose the induced changes of shock. The fall in MAP and pulse pressure reduces the stimulation of the high-pressure baroreceptors in the carotid sinus and the aortic arch. The negative stimulation of the cardiovascular control centres in the brainstem enhances the sympathetic tone (and reduces the vagal tone) leading to increased heart rate and contractility as well as to arteriolar and venous constriction mainly in the skin, skeletal muscles and the splancnic area. The bloodflow favours the brain and the heart as long as possible. An array of other compensatory reactions are given in Fig. 12-6: Increased vascular permeability, reduced capillary pressure with autotransfusion from the interstitial fluid, thirst and drinking followed by absorption of fluid from the gastrointestinal tract, and release of powerful vasoconstrictors such as adrenaline, angiotensin II, vasopressin etc. Catecholamines and enkephalins are released from chromaffine granules in the adrenal medulla. Catecholamines increase the heart rate and the cardiac output by stimulation of the adrenergic b1-receptors in the myocardium. Catecholamines constrict vessels all over the body by stimulating a1-receptors located on the surface of vascular smooth muscles. ADH (vasopressin) is secreted from the posterior pituitary gland in response to shock, because the sinoaortic baroreceptors are under-stimulated. Vasopressin is a modest vasoconstrictor and a strong antidiuretic hormone. The increased ADH secretion causes increased fluid reabsorption by the kidneys and restores blood pressure and volume. Renin is secreted from the juxtaglomerular apparatus, when blood pressure and renal perfusion falls drastically. Renin acts on the plasma protein, angiotensinogen, to form inactive angiotensin I, which is transformed to the powerful vasoconstrictor, angiotensin II by angiotensin converting enzyme, ACE. The most likely trigger of the renin-angiotensin-aldosterone cascade is described in Chapter 24. - The rise in normal plasma-[K+] due to the ischaemia of shock also releases aldosterone. ACTH and b-endorphins are released into the blood from the anterior pituitary gland Chapter 26) in response to haemorrhage or other forms of stress. ACTH and endorphins both exaggerates and restricts the development of shock. These opioids depress the brainstem control centres that normally mediate autonomic responses to stress. Hence, naloxone (an opioid antagonist) improves the circulation and increases the rate of survival from life-threatening shock. - On the other hand, ACTH has a small aldosterone and a strong cortisol stimulating effect. Initially, the bleeding patient suffers from hypercoagulability. Thromboxane A2 (TxA2) aggregates thrombocytes, and the aggregate releases more TxA2. This positive feedback prolongs the clotting tendency. In this phase anticoagulants (heparin) reduce the mortality from shock. Fig. 12-6: Development of shock conditions. Effects, effectors and reactions are shown. 1B. Serious shock leads to myocardial damage, because the arterial pressure is too low to secure a coronary bloodflow adequate for nutrition. Myocardial contractility is depressed, and the ventricular function curve shifts to the right (Fig. 10-5B). Loss of more than 35% of the total blood volume of a healthy person is a threat, if the loss is unaided by blood transfusion. An arterial blood pressure below 8 kPa, where there is no additional baroreceptor response can stimulate the chemoreceptors of the carotid body and increase ventilation. The sucking effect of the low inspiratory pressure improves the venous return to the heart. Cerebral ischaemia is consequential at arterial pressures below 5 kPa. The cerebral hypoxia elicts a generalised and powerful sympathetic stimulation with a pronounced arteriolar-and venous-constriction. Further hypoxia in the brainstem activates the vagal centres resulting in bradycardia. 1C. Irreversible shock is a terminal condition, where all therapy is frustraneous. Nothing can save the patient. The progressive deterioration becomes irreversible at a blood loss of more than 50% of the total blood volume. The drastic fall in arterial blood pressure reduces the renal glomerular filtration pressure below the critical level, so filtration is diminished or abolished, leading to abolish urine output (anuria). The low cardiac output and bloodflow result in stagnant hypoxia of all mitochondria. Hypoxia increases lactic acid liberation. Renal failure with tubular necrosis prevents excretion of excess H+. The high H+-concentration further depresses the myocardium, reduces blood pressure and thus the tissue bloodflow. This aggravates the metabolic acidosis - a classical vicious cycle (Fig. 12-6). In the later stage of haemorrhagic shock, there is fibrinolysis and prolonged coagulation time (hypocoagulability). Hence, heparin therapy can be lethal. The phagocytic activity of the reticulo-endothelial system (RES) is depressed during shock. Endotoxins constantly enter the blood from the bacterial, intestinal flora of a healthy person. The macrophages of the RES (Chapter 32) normally inactivate these endotoxins and release mediators such as hydrolases, proteases, oxygen free radicals, coagulation factors, prostaglandins, thromboxanes and leucotrienes. Some of these mediators modulate the temperature control and hormone secretion. Following loss of half the total blood volume the shock patient must have lost about 50% of his circulating macrophages, and control substances modulating the phagocytic activity of RES. The depressed defence mechanisms in RES result in an endotoxic shock which aggravates the haemodynamic shock - a vicious cycle. The patient loose consciousness and falls into a state of stupor or of coma. A severe shock becomes irreversible, when the high-energy phosphate stores of the liver and heart are depleted. All of the creatine phosphate is degraded and almost all ATP has been degraded to ADP, AMP and eventually to the even more efficient vasodilatator, adenosine. Adenosine diffuses out of the cells and into the circulation, where it is converted into hypoxanthine and uric acid, a substance that cannot re-enter the cells. Cellular depletion of high-energy phosphate is probably causing the final state of irreversibility. The cerebral bloodflow is now so low that the function of the cardiovascular brainstem centres is depressed. The loss of sympathetic tone leads to cardiac depression with terminal bradyardia and vasodilatation with falling peripheral resistance. The fall in arterial pressure intensifies the damage, and a vicious cycle is established. Two types of shock deserve special consideration: Anaphylactic shock (anaphylaxis with relative hypovolaemia) is a severe allergic disorder in which the cardiac output and the mean arterial pressure fall rapidly and drastically due to relative hypovolaemia. As soon as an antigen to which the patent is sensitive, has entered the blood the antigen-antibody reaction (Chapter 32) triggers release of histamine from basophilic cells in the blood and mast cells in the tissues. Histamine dilatates arterioles and most peripheral vessels. This results in falling arterial pressure and increased capillary permeability with rapid loss of plasma water into the interstitial fluid. Septic shock (relative hypovolaemia). Septic shock or blood poisoning is a widespread bloodborn bacterial infection - often life threatening. Examples are gas gangrene bacilli spreading from a gangrenous limb, colon bacilli with endotoxin spreading into the blood from infected kidneys (pyelonephritis), and fulminant peritonitis due to acute abdominal disease. Frequent causes of fulminant peritonitis are rupture of the infected gut or the uterus, and rupture of the uterine tube due to extrauterine pregnancy. Septic shock is characterized by tremendously high fever, high cardiac output, marked vasodilatation, red cell agglutination, disseminated intravascular coagulation withmicroclots spread all over the circulatory system. When the clotting factors are used up, internal haemorrhages occur. Endotoxins produce vasodilatation, induce synthesis of nitric oxide (NO) synthase in the vascular smooth musculature. Overproduction of NO may contribute to the vasodilatation and the depressed myocardial contractility found in septic shock. The high cardiac output is due to a high stroke volume and a high heart rate. The diastolicpressure is low and the systolic pressure is high until endotoxins begin to inhibit myocardial contractility seriously. Now the condition is in a vicious cycle, which is often fatal. Therapy keypoints are: First of all the cause has to be established in order to give the appropriate therapy. 1. Head-down position (placing the patient’s head below the level of the heart) is the immediate therapy of haemorrhagic and neurogenic shock. 2. Haemorrhagic arrest (closing the abdominal aorta with the pressure of a fist, or blocking the bleeding from an artery with a finger) is often life saving when applied without unnecessary delay. 3. Replacement transfusions. The best possible therapy of haemorrhagic shock is whole blood transfusion. The best treatment of shock caused by plasma loss is plasma transfusion, and the best therapy of dehydration shock is transfusion with the appropriate solution of electrolytes. 4. Oxygen breathing is always helpful in shock with insufficient delivery of oxygen.
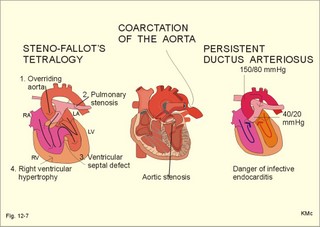
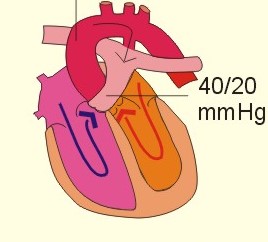
On a global scale approximately 1% of live births result in congenital heart disease. The mother may have suffered from rubella infection, abuse of drugs or alcohol, exposure to influential radiation or other factors causing genetic or chromosomal abnormalities. Two pathophysiological phenomena occur: Right-to-left shunting of blood results in cyanosis, clubbing of fingers, reduced growth in children, exertion syncope, and paradoxical emboli from veins to systemic arteries. Children with Steno-Fallot´s tetralogy (Fig. 12-7) use squatting. The advantage of squatting for the children is improved cerebral oxygenation as the position reduces the right-to-left shunt. Left-to-right shunts in the heart result in pulmonary hypertension, because of persistently increased pulmonary bloodflow and vascular resistance (the so-called Eisenmenger response - frequently caused by ventricular septal defect). Three classical congenital heart diseases are Steno-Fallot´s tetralogy, Coarctation of the aorta, and persistent ductus arteriosus. The four elements suggested by the name tetralogy are: 1. Ventricular septal defect, 2. Overriding aorta (ie, the aortic orifice is located above the ventricular septal defect and therefore receives blood from both ventricles), 3. Pulmonary stenosis (right ventricular outflow obstruction), and 4. Right ventricular hypertrophy. The pulmonary stenosis causes a high right ventricular pressure, and as this pressure supersedes the left ventricular pressure there is a right-to-left shunting of blood through the ventricular septal defect. The mixed blood passes through the overriding aorta, and the patient is cyanotic with all the hypoxic consequences described above (eg, exertion syncope, squatting, small stature, finger clubbing and polycythaemia). The children are tired and dyspnoeic, and growth is retarded although they often demonstrate a surprising appetite, because of the enormous cardiac work. Complete surgical correction is possible. Fig. 12-7: Three common congenital heart disorders. Coarctation is a narrowing of the aorta distal to the insertion of ductus arteriosus (Fig. 12-7), and often associated with stenosis of the aortic orifice (a bicuspid aortic valve). The obstructed aortic bloodflow forces blood through collateral arteries such as the intercostal and periscapular arteries. The high blood pressure may cause nose bleeds and headaches, and the low distal bloodflow may cause claudication and cold legs. Turbulent bloodflow through the coarctation is often recognized as a forceful systolic murmur even on the back. Surgical excision of the coarctation with end-to-end anastomosis must be performed in childhood, because a low renal bloodflow, maintained over years, frequently results in irreversible systemic hypertension Persistent ductus arteriosus (PDA) In the foetus the ductus arteriosus leads blood into the systemic circulation instead of through the unexpanded lungs. Hereby, the foetal blood is oxygenated during its passage of the placenta. At birth, the expansion of the lungs with atmospheric air triggers contraction and closure of ductus arteriosus by constriction of its muscular wall. Premature babies and children borne by mothers, who suffered from rubella in the first trimester, are often born with PDA. A PDA shunts blood from the aorta to the pulmonary artery throughout the cardiac cycle (Fig. 12-7). This is because the aortic pressure is much higher (150/80 mmHg) than that of the pulmonary artery (40/20 mmHg or 5.3/2.7 kPa). The condition may be symptom-less for years, but a large shunt increases the work of the left ventricle and causes left heart failure, which increases the risk of pulmonary congestion and oedema. The person is easily fatigued even from moderately strenuous exercise. The frequency of infective endocarditis is increased in PDA. Infective endocarditis commonly occurs on congenitally or rheumatically damaged valves. The endocardium also suffers from jet lesions located on the endocardial surface opposite to a shunt with a high driving pressure. This is common for all types of congenital heart disease apart from atrial septal defect, where the driving shunt pressure is too small to damage the endocardium. The continuous shunting of turbulent blood causes a continuous machinery murmur best heard below the left clavicle. Surgical ligation of the duct should be performed as early as possible. The general trend today is an increasing survival rate of congenital heart disease. Adults living with congenital heart disease for years may present themselves as cardiac arrhythmias resistant to standard therapy or at autopsy following sudden cardiac death. Terminal heart failure is now managed by heart-lung transplantation. · The Fick cardiac output equation states that the cardiac output is calculated from the ratio between alveolar oxygen uptake and arteriovenous oxygen content difference: Eq. 12-1: Q° = V° O2/(CaO2 - Cv O2 ); [ml STPD*min-1/ml blood*min-1]. The last oxygen concentration is in mixed venous blood. · The law of mass balance is applied to both bloodflow and oxygen flux in Eq. 14-7 and 14-8. The flow and flux relations implies the following shunt equation: Eq. 12-2: Q°shunt/ Q°total = (CaO2 - Cc´02)/(Cv O2 - Cc´02).The last oxygen concentration is in pulmonary end-capillary blood. · Clearance is the volume of blood plasma, which is totally cleared each minute of a given indicator by a specific organ (renal clearance). The extraction (E) is the fraction of substance that is extracted from the total amount transported to the organ per minute. Eq. 12-3: E = Q° (Ca - Cv) /( Q° × Ca) ; E = (Ca - Cv) / Ca · The isotope-wash-out-method. A homogenous muscle tissue of the weight, Wtis, is presumed. A lipid-soluble indicator such as 133Xenon dissolved in saline, is injected in the tibialis anterior muscle (* in Fig. 12-4). At steady state, the tracer concentration in the venous blood (Cv) is assumed to be the average blood concentration, and Ctis the mean tissue concentration. A distribution coefficient is introduced: Ctis/Cv = l, which is known for Xenon. The decrease of the mass of indicator in the tissue per time unit (dt) must be equal to the mass supplied (which is zero) minus the mass of indicator leaving the tissue in the venous blood. The principle of mass balance provides the following equation: (Wtis × dCtis) = [mass supplied minus mass eliminated]. (Wtis × dCtis) = (- Cv × Flow× dt) or Wtis × dCtis/Ctis = (- Cv/Ctis × Flow × dt). Eq. 12-4: dCtis/Ctis = - Flow × dt/(Wtis × l). The fractional fall in the mean tissue concentration of Xenon (Ctis) per time unit (dt) is constant during the whole elimination period (a rate constant = ln 2/T½). Flow/Wtis is a perfusion coefficient in FU (ml of blood per min and per 100 g tissue). The ratio dCtis/Ctis is measurable as T½ on the skin surface above the Xenon deposit in fat or muscle tissue with a scintillation detector. · The volume equation for a cylindrical system implies that the flow per second (Q° s) and its volume (V) is related by tmean: Eq. 12-5: tmean = V/ Q°s. I. Each of the following five statements have True/False options: A. The capillaries have the greatest cross-sectional area of the systemic circulation. B. The systemic arterioles offer the greatest vascular resistance to bloodflow. C. The sympathetic regulation of the arteriolar tone in fat and skin tissue depends upon the classical baroreceptors. D. Increased compliance in the venous system means decreased venous return. E. The lactate produced by skeletal muscles during exercise is not an important substrate for the myocardial metabolism. II. Each of the following five statements have True/False options: A. Vasopressin is a strong antidiuretic hormone and a modest vasoconstrictor. B. ACTH and b-endorphins are released into the blood from the posterior pituitary gland in response to haemorrhage or other forms of stress. C. Fulminant peritonitis is a frequent form of acute abdominal disease. D. With the head of the patient downward, the patient risks air embolism if blood vessels are cut during neck and head surgery. E. Hypotension and ischaemic hypoxia depresses myocardial contractility. 20-year old soldiers, body weight 70 kg, is brought to the field hospital with a profusely bleeding gun wound in the left shoulder. The skin is cold and wet, the arterial pressure is 65/ 40 mmHg, and the heart frequency is 144 beats per min (bpm). There is no diuresis. The bleeding is stopped by ligation of the bleeding arteries, and blood transfusions are given instantly (2 litres of whole blood with a normal packed cell volume, PCV, of 0.45). Hereby, the arterial pressure increases to a steady level of 105/70 mmHg, and the heart rate is reduced to 100 bpm. The condition of the soldier is clearly improved and his cardiac output is measured to 3.5 l per min. 24 hours later the soldier had a relapse, and his PCV was measured to 0.35. The PCV is corrected for trapped plasma, and assumed representative for the body as a whole (ie whole body haematocrit). 1. Describe the initial cardiovascular events leading to the shock condition. 2. Describe the effect of the blood transfusions. 3. Calculate the order of size of the blood loss. 4. Was the blood transfusion therapy sufficient? A male, 21 years old, is located in the supine body position. He has a cardiac output of 5.4 l per min at rest, a circulating blood volume in the pulmonary circulation of 650 ml and in the systemic circulation of 4750 ml. His total mass of skeletal muscle is 35 kg. The muscular perfusion is 3 ml of blood per min per 100 g of muscle tissue (3 FU), and the mean passage time in the muscular capillaries is 5 s. 1. Calculate the mean transit time for all red blood cells in the total circulatory system. 2. Calculate the mean transit time for the pulmonary circulation only. 3. Calculate the total perfusion of the skeletal muscle mass at rest (ml/min) and calculate the bloodflow per second. 4. Calculate the functioning capillary volume in the muscular capillaries. A 64-year old male normally has a body weight of 74 kg, a total blood volume of 5 l and a blood [haemoglobin] of 10 mmol per l (mM). One day he suddenly vomits large quantities of fresh blood. For two days his stools have been tarry. The last weeks have been stressful at work. The patient calls his doctor and the emergency ward at the hospital is alerted. Due to an incompetent local ambulance service, the patient is brought to hospital without delay by taxi. Here, the mean arterial blood pressure is below 10 kPa (75 mmHg) and falling. The heart rate is above 150 beats per min and rising. The blood [haemoglobin] is 5 mM measured one hour after the first massive blood loss. The emergency team immediately institute transfusion of blood. The following 8 days the patient receives three transfusions of blood and at least 10 l of physiological saline. On the second day his [haemoglobin] has increased to 7.2 mM, but on the third day it falls again to 5 mM. On the 4th day at the hospital the patient develops high fever (maximum 40.6 oC), and a broad-spectrum antibiotic program is started without delay. On the 8th day at hospital the patient has normal temperature, but he develops watery swellings of legs and lower abdomen, in spite of pronounced urination. The body weight is now 80 kg. 1. What is the most likely cause of the haemorrhage? 2. Estimate the size of his blood loss. 3. Why did the patient develop high fever? 4. Why did the patient accumulate water? A small girl, borne with ventricular septal defect, pulmonary stenosis, overriding aorta and a right to left shunt through the septal defect is examined with cardiac catheterisation. The oxygen concentrations in her blood are 138, 195, and 220 ml per l in the pulmonary artery, brachial artery and pulmonary veins, respectively. Her oxygen uptake at rest is 164 ml per min, and she has polycythaemia with a blood haemoglobin of 164.2 g per l. The girl has a 30% right-to-left shunt through the septal defect and directly to the overriding aorta. 1.What is the diagnosis? 2. Calculate the oxygen concentration in the pulmonary veins and estimate the saturation degree. 3. Calculate the bloodflow through the lungs. 4. Calculate the total bloodflow through the aorta assuming that the lung bloodflow (Q°lung ) and the shunt bloodflow (Q°shunt ) equals the total cardiac output, Q°total . 5. Estimate the size of the venous return. 6. Is it likely that this patient develops cyanosis? Calculate the concentration of reduced haemoglobin in mean capillary blood. A male, 18 years old, suspect of congenital heart disease, is examined at the hospital. His body weight is only 60 kg and he has always abstained from exercise. The patient is tall and slim, although he is always hungry and is actually eating more than normal. Cardiac catheterisation is performed with the patient resting in the supine position, and reveals the following: Mixed venous blood from the right ventricle and from the pulmonary artery (CvO2 ): 160, arterial blood from the aorta (CaO2 ) 195, and blood from the right atrium 130 ml STPD l-1. The oxygen uptake (V°O2 ) at rest is 310 ml STPD per min. 1. Calculate the cardiac output (Q°) from the right ventricle. 2. Calculate the Q° from the left ventricle. 3. Provide arguments for a certain cardiac abnormality, which explains the findings. 4. Why has the patient always avoided exercise? 5. Why is the patient slim although he is eating a lot and not performing exercise? Try to solve the problems before looking up the answers. · The coronary bloodflow is mainly controlled by local metabolic autoregulation. Accordingly, a moderate decrease in arterial blood pressure down to 9.3 kPa (70 mmHg) does not significantly reduce the bloodflow through the myocardium. · The blood reaches the brain through the internal carotid and the vertebral arteries. The dominant control of cerebral bloodflow (CBF) is autoregulation. The sympathetic nervous system plays a secondary role. · Some degree of autoregulation is found in many other organs including the skeletal muscle mass, the splancnic area, and the kidneys. · CBF is normally 55 FU in humans at rest. One Flow Unit (FU) is one ml of blood per min per 100 g of brain tissue. This resting CBF and the oxygen uptake of the brain can double during cerebral activity and triple in active brain regions during an epileptic attack. Brain vessels are metabolically regulated. Increased PaCO2, and reduced PaO2 dilatate brain vessels and increase CBF. · Blood flows through the skin and subcutaneous tissues in order to nourish the cells, and to regulate shell temperature. Blood flows much faster through the arteriovenous anastomoses in the skin of the face, the fingers and toes in a cold environment. The sympathetic activity constricts the metarterioles that lead to the skin, so the blood bypasses the cutaneous circulation. · Psychological influence can cause one to blush or to have a white face, by changing a-adrenergic constrictor tone and via the effect of local, vasoactive substances normally found in the skin. · When a large fat combustion is occurring (eg, hunger and distance running), the fat bloodflow can increase from 3 FU to 20 FU. Cold and warm environments alter the fat perfusion just like the skin perfusion. · The placental barrier has an area of 10 m2, and can be passed by low molecular substances (nutrients, gasses, and waste) by diffusion. The foetal haemoglobin (F) has a dissociation curve that is shifted to the left relative to adult haemoglobin, and F is not affected by 2,3-DPG.. · Foetal blood has a high haemoglobin concentration, so the foetus takes up large amounts of O2 in placenta. · Much of the blood flowing in the descending aorta of the foetus is directed toward the placenta, so venous drainage from all organs is shunted toward the placenta, where wastes are eliminated from foetal blood, whereas O2 and nutrients are acquired. · The parallel foetal circulation is transformed into a series circulation in the baby. The foramen ovale and ductus venosus close within 3 days of birth, and the ductus arteriosus closes within 10 days. The sharp increase of O2 content (CaO2) in the baby's blood is a potent and universal vasodilatator. The dramatic changes in gas exchange affect cardiopulmonary and vascular regulation, probably via local mediators such as arachidonic acid and prostacyclin. · When a supine person arise, his TPVR increases, the systolic blood pressure falls and the diastolic blood pressure rises. Thus the pulse pressure amplitude falls, the MAP is unchanged. The stroke volume is reduced more than the heart rate rises, so the cardiac output will decrease in the standing position. · The bloodflow (cardiac output in ml of blood per s or more convenient per min) can be measured by dividing the dose of indicator injected upstream by the area under the downstream concentration curve. · Clearance is the volume of blood plasma. Which is totally cleared each minute of a given indicator by a specific organ. · Catecholamines constrict vessels all over the body by stimulating a1-receptors located on the surface of vascular smooth muscles. · ADH (vasopressin) is secreted from the posterior pituitary gland in response to shock, because the sinoaortic baroreceptors are under-stimulated. Vasopressin is a modest vasoconstrictor and a strong antidiuretic hormone. · The enzyme renin is secreted from the juxtaglomerular apparatus, when blood pressure and renal perfusion falls drastically. Renin acts on the plasma protein, angiotensinogen, to form inactive angiotensin I, which is converted to the powerful vasoconstrictor, angiotensin II by ACE in the lungs. · Angiotensin II is a powerful stimulator of the aldosterone secretion from the renal cortex. Aldosterone promotes the reabsorption of Na+ and increases the secretion of K+ and H+ in the distal tubular system of the kidneys. Water follows by osmosis, so the extracellular volume is increased. · ACTH and b-endorphins are released into the blood from the anterior pituitary gland in response to haemorrhage or other forms of stress. · Septic shock or blood poisoning is a widespread bloodborn bacterial infection - often life-threatening. Examples are gas gangrene bacilli spreading from a gangrenous limb, colon bacilli with endotoxin spreading into the blood from infected kidneys, and fulminant peritonitis due to acute abdominal disease. · Haemorrhagic arrest (haemostasis) is often life saving in shock, when applied without unnecessary delay. · Replacement transfusions. The best possible therapy of haemorrhagic shock is whole blood transfusion, of shock caused by plasma loss plasma transfusion, and of dehydration shock transfusion with the appropriate solution of electrolytes. · Oxygen breathing is helpful in shock with insufficient delivery of oxygen. · Sympathomimetic drugs (noradrenaline, adrenaline etc) are often beneficial in neurogenic and anaphylactic shock. They are seldom useful in haemorrhagic shock. Calver, A., J. Collier and P. Vallance. "Nitric oxide and cardiovascular control." Experimental Physiology 78: 303-326, 1993.
|
||
Click here to introduce your comments or contributions